Pain patches have become a powerful and convenient method for managing chronic and acute pain. They deliver medication slowly through the skin, offering long-lasting relief with fewer peaks and valleys compared to pills. Because they involve potent medications—especially opioids like fentanyl—every registered nurse must understand proper handling, safety precautions, and patient education. This topic appears frequently on the NCLEX, making it essential for every RN nurse and nursing student to master.
Whether used in hospitals, rehabilitation centers, or at home, pain patches require careful assessment and monitoring. A strong grasp of these nursing responsibilities can easily become part of a nursing bundle focused on medication safety.
What Are Pain Patches?
Pain patches are transdermal systems designed to release medication steadily over hours or days. Common examples include:
- Fentanyl patches (opioid analgesic)
- Lidocaine patches (local anesthetic)
- Diclofenac patches (NSAID)
- Buprenorphine patches
- Capsaicin patches
Each one has specific dosing intervals, safety instructions, and monitoring priorities that the nurse must understand to avoid toxicity or treatment failure.
Nursing Responsibilities When Handling Pain Patches
1. Ensuring Proper Patch Placement
A registered nurse must apply the patch to clean, dry, intact skin—never on irritated or broken skin. Hair should be clipped, not shaved, to prevent micro-abrasions. Rotating sites reduces the risk of skin irritation.
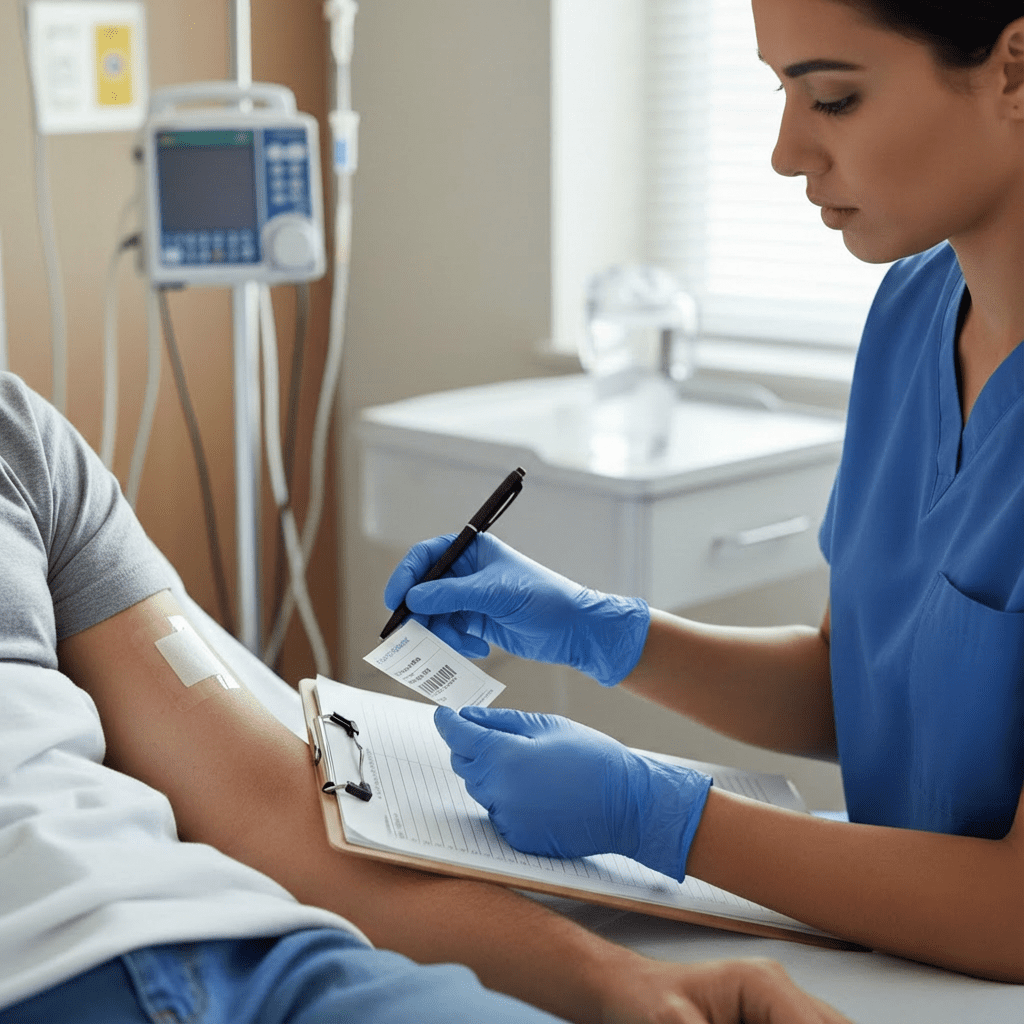
2. Documenting and Tracking Patches
Fentanyl and buprenorphine patches require strict tracking because they contain dangerous amounts of medication. Every RN nurse documents:
- Time of application
- Patch location
- Removal time
- Disposal method
Accurate documentation prevents double dosing and medication errors—a major NCLEX focus.
3. Assessing for Effectiveness and Side Effects
After applying a pain patch, nurses monitor:
- Pain level
- Respiratory status (especially with opioids)
- Skin integrity
- Mental status
- Signs of overdose
Because transdermal medications absorb slowly, effects may take several hours. A nurse must teach patients not to expect immediate relief with certain patch types.
Safety Considerations for Pain Patches
1. Heat Exposure
Heat dramatically increases absorption of opioid patches. This puts the patient at risk for respiratory depression. Nurses must teach patients to avoid:
- Heating pads
- Sunbathing
- Hot tubs
- Fever (notify provider)
This topic appears frequently in NCLEX pharmacology questions.
2. Cutting Patches
Most patches cannot be cut, because doing so disrupts controlled release and may cause toxicity. A registered nurse must understand which patches are safe to cut (very few) and which are not.
3. Secure Disposal
Pain patches must be folded with the sticky sides together and disposed of in medication waste containers or flushed (depending on hospital policy). A used fentanyl patch still contains enough medication to cause overdose in children or pets.
4. Avoiding Accidental Transfer
Patients should never touch the medication side of the patch and should wash hands after application. Skin-to-skin contact may accidentally transfer medication to someone else, especially with opioid patches.
Essential Patient Teaching for Pain Patches
RN nurses play a critical role in teaching patients how to use patches safely. Education may include:
1. When and How to Apply Patches
- Apply at the same time of day
- Rotate sites
- Avoid placing on hairy or irritated skin
- Press firmly for 30 seconds
2. How to Recognize Overdose or Toxicity
Especially with fentanyl:
- Extreme sleepiness
- Slow breathing
- Blue lips or nails
- Confusion
- Pinpoint pupils
Every nurse must act quickly, call emergency services, and remove the patch if overdose is suspected.
3. What to Do If a Patch Falls Off
Patients should:
- Apply a new patch
- Document the time
- Notify the provider (especially for opioids)
4. Limitations of Pain Patches
Nurses explain that patches:
- Do not provide rapid pain relief
- Do not replace short-acting medications for breakthrough pain
- Require continuous monitoring
This helps patients develop realistic expectations and improves adherence.
Final Thoughts
Pain patches provide powerful pain control when used safely, but they require strong nursing assessment, accurate documentation, patient teaching, and ongoing monitoring. Because of their potency and long duration, these patches remain a high-priority topic on the NCLEX, especially regarding opioid safety.
FAQ
Yes, most patches are waterproof. They should avoid scrubbing or putting lotion on the site.
No. Heat increases absorption and can cause overdose—especially with fentanyl patches.
Patients should not replace it without calling their RN or provider. The dose may need adjustment.
Never—except lidocaine when ordered. Cutting opioid patches can release too much medication at once.