Cardiac medications are a high-yield topic on the NCLEX and a daily reality for every nurse working in med-surg, critical care, or primary care. As a registered nurse (RN nurse), you must be able to identify drug classes, their mechanisms, side effects, and key patient teaching points. This quick guide breaks down beta blockers, ACE inhibitors, and diuretics—three medication classes you’ll encounter often in clinical practice and on the exam.
🔹 Beta Blockers (“-olol” Drugs)
Examples: Metoprolol, Atenolol, Propranolol
Mechanism:
- Block beta-adrenergic receptors → slow heart rate, reduce cardiac output, lower blood pressure.
Indications:
- Hypertension
- Heart failure (selective beta blockers)
- Angina
- Post-MI protection
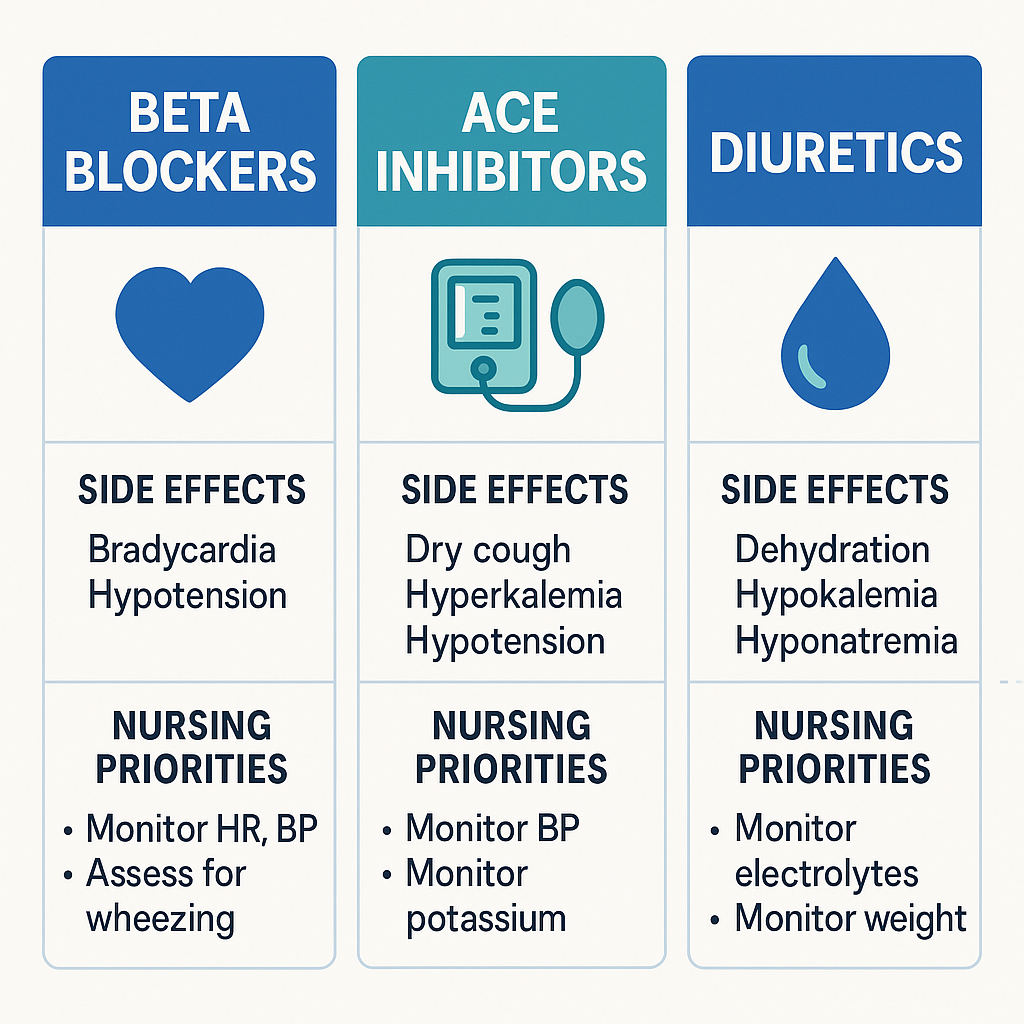
Nursing Considerations:
- Monitor HR and BP before administration (hold if HR < 60 bpm).
- Can mask signs of hypoglycemia—important for diabetic patients.
- Avoid abrupt withdrawal (risk of rebound hypertension and angina).
💡 NCLEX Tip: Think “LOL makes the heart slow.”
🔹 ACE Inhibitors (“-pril” Drugs)
Examples: Lisinopril, Enalapril, Captopril
Mechanism:
- Inhibit angiotensin-converting enzyme → block conversion of angiotensin I to angiotensin II → vasodilation and reduced blood pressure.
Indications:
- Hypertension
- Heart failure
- Post-MI care
- Diabetic nephropathy
Nursing Considerations:
- Monitor for dry cough (classic side effect).
- Watch for angioedema (airway emergency).
- Monitor potassium (risk of hyperkalemia).
- Assess kidney function (BUN, creatinine).
💡 NCLEX Tip: Think “ACE = Angioedema, Cough, Electrolytes (K+).”
🔹 Diuretics
Loop Diuretics (e.g., Furosemide/Lasix):
- Powerful, used for fluid overload, CHF, pulmonary edema.
- Nursing priorities: Monitor potassium (risk of hypokalemia), daily weights, strict I&O, assess for ototoxicity.
Thiazide Diuretics (e.g., Hydrochlorothiazide):
- Used for hypertension, mild fluid overload.
- Monitor electrolytes, especially sodium and potassium.
Potassium-Sparing Diuretics (e.g., Spironolactone):
- Used in CHF and hypertension.
- Watch for hyperkalemia, especially when combined with ACE inhibitors.
💡 NCLEX Tip: Remember “Diuretics = Diet & Daily Weights.”
🩺 Nursing Priorities for Cardiac Meds
For all three drug classes, nursing care focuses on:
- Monitoring vital signs (BP, HR, respiratory status).
- Checking electrolytes (K+, Na+, renal labs).
- Watching for orthostatic hypotension and fall risk.
- Educating patients on adherence, diet modifications, and when to report adverse effects.
Why Nurses Must Master Cardiac Meds
Whether you’re a student preparing for the NCLEX or a registered nurse at the bedside, cardiac medications are non-negotiable knowledge. From understanding drug suffixes to knowing which lab values to monitor, mastering these meds boosts your confidence in patient safety and exam performance.
For a deeper dive into cardiac care, check out a nursing bundle that organizes meds, labs, and interventions into simplified study sheets.
✅ Final Takeaway:
- Beta Blockers: Slow HR & BP, monitor for bradycardia and masking of hypoglycemia.
- ACE Inhibitors: Lower BP, watch for cough, angioedema, hyperkalemia.
- Diuretics: Reduce fluid overload, monitor electrolytes and kidney function.
These three cardiac med classes will follow you from nursing school to daily practice.