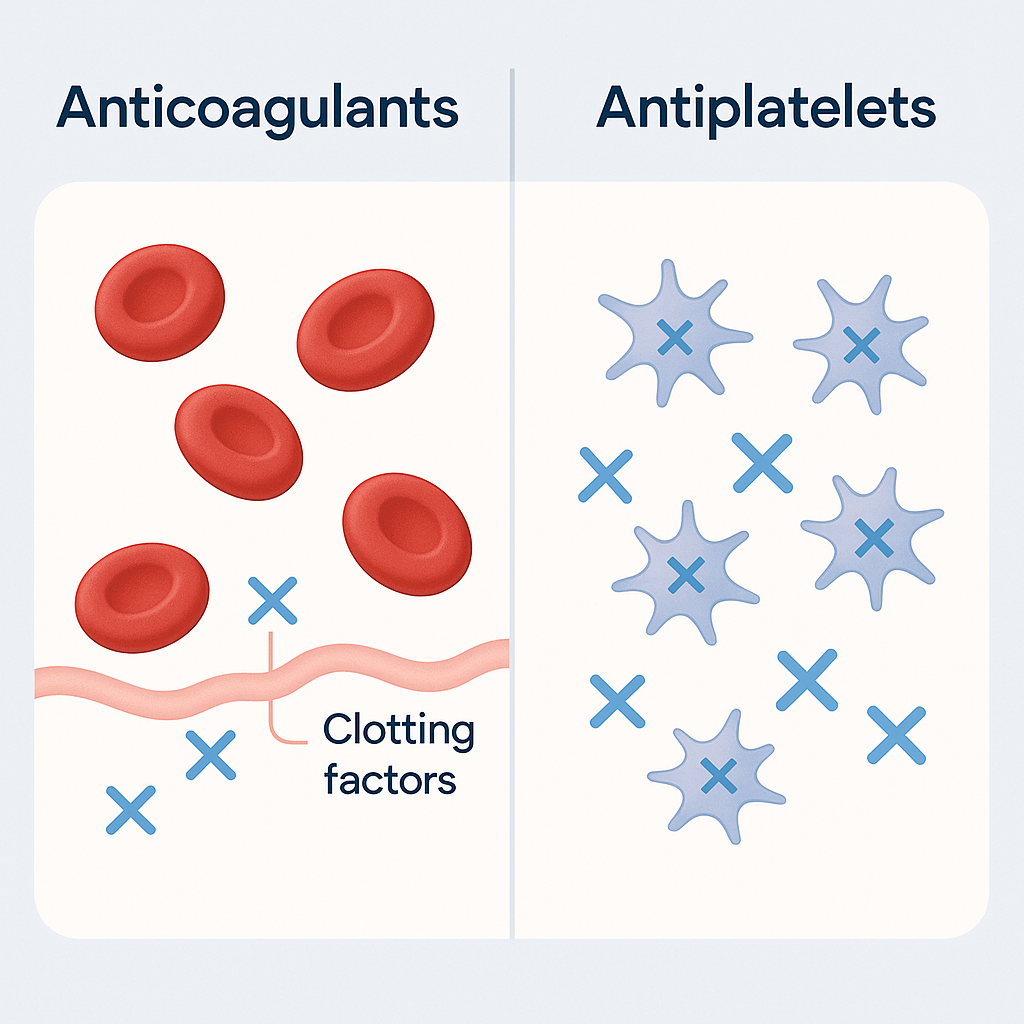
When preparing for the NCLEX, nurses often find themselves reviewing cardiovascular medications. Among the most frequently tested topics are anticoagulants vs antiplatelets. While both are used to reduce the risk of blood clots, their mechanisms, uses, and nursing considerations are different. Every registered nurse (RN nurse) should understand these distinctions to provide safe and effective patient care.
What Are Anticoagulants?
Anticoagulants are medications that slow down the clotting process by interfering with the clotting cascade. They are sometimes referred to as “blood thinners,” but they don’t actually thin the blood — they prevent new clots from forming and stop existing ones from getting bigger.
Common Examples
- Warfarin (Coumadin)
- Heparin (unfractionated)
- Enoxaparin (Lovenox – low molecular weight heparin)
- Apixaban (Eliquis), Rivaroxaban (Xarelto) – newer oral anticoagulants
Nursing Notes for Anticoagulants
- Monitor INR/PT for warfarin and aPTT for heparin.
- Watch for signs of bleeding: bruising, nosebleeds, bloody urine or stools.
- Teach patients on warfarin about vitamin K interactions (leafy greens).
- Emphasize safety: use soft toothbrushes, electric razors, and avoid high-risk activities.
What Are Antiplatelets?
Antiplatelets work by preventing platelets from clumping together to form clots. They are most commonly prescribed for patients with atherosclerosis, heart attack, or stroke prevention.
Common Examples
- Aspirin (ASA)
- Clopidogrel (Plavix)
- Ticagrelor (Brilinta)
Nursing Notes for Antiplatelets
- Monitor for GI upset and bleeding.
- Instruct patients to report black/tarry stools or unusual bruising.
- Use cautiously with other drugs that increase bleeding risk (NSAIDs, anticoagulants).
- Important for post-stent and post-MI patients.
Anticoagulants vs Antiplatelets – Key Differences
| Feature | Anticoagulants | Antiplatelets |
|---|---|---|
| Mechanism | Interfere with clotting factors in the clotting cascade | Prevent platelet aggregation |
| Examples | Warfarin, Heparin, Apixaban | Aspirin, Clopidogrel |
| Monitoring | INR, aPTT (depending on drug) | No routine lab monitoring |
| Primary Use | DVT, PE, atrial fibrillation, mechanical heart valves | Stroke prevention, post-MI, stent placement |
| Reversal | Vitamin K (warfarin), Protamine (heparin) | No specific antidote (manage bleeding supportively) |
NCLEX Nursing Tips
- Expect NCLEX questions asking: Which lab value do you check for a patient on warfarin? or What patient teaching is priority for someone starting aspirin therapy?
- Remember: Anticoagulants = clotting factors, Antiplatelets = platelet stickiness.
- Always think about bleeding risks and patient safety when answering NCLEX questions related to these meds.
Why This Matters for Nursing Practice
Every nurse must be confident in distinguishing between these two classes of drugs. Whether you’re a registered nurse in the hospital setting, preparing for the NCLEX, or reviewing with a nursing bundle for pharmacology, understanding anticoagulants vs antiplatelets is vital for preventing complications and ensuring patient safety.
✅ Final Note for RN Nurses: Keep it simple —
- Anticoagulants = clotting cascade.
- Antiplatelets = platelet aggregation.
Both require vigilance, patient education, and strong clinical judgment.