Understanding insulin types is essential for every nurse, especially those preparing for the NCLEX or working directly with patients who have diabetes. Because insulin therapy can prevent life-threatening complications, registered nurses and RN nurses must recognize how onset, peak, and duration influence blood glucose control. This guide provides a simplified, student-friendly breakdown to support your clinical practice and complement your nursing bundle study resources.
✅ Why Nurses Must Understand Insulin Pharmacokinetics
Safe insulin administration requires more than memorizing names. Nurses must know when each insulin starts working, when hypoglycemia is most likely, and how long the medication stays active.
Moreover, this knowledge helps a nurse:
- Adjust insulin around meals
- Prevent hypoglycemia
- Provide accurate patient education
- Respond quickly to glucose emergencies
For NCLEX success and real-world practice, this is a foundational pharmacology skill.
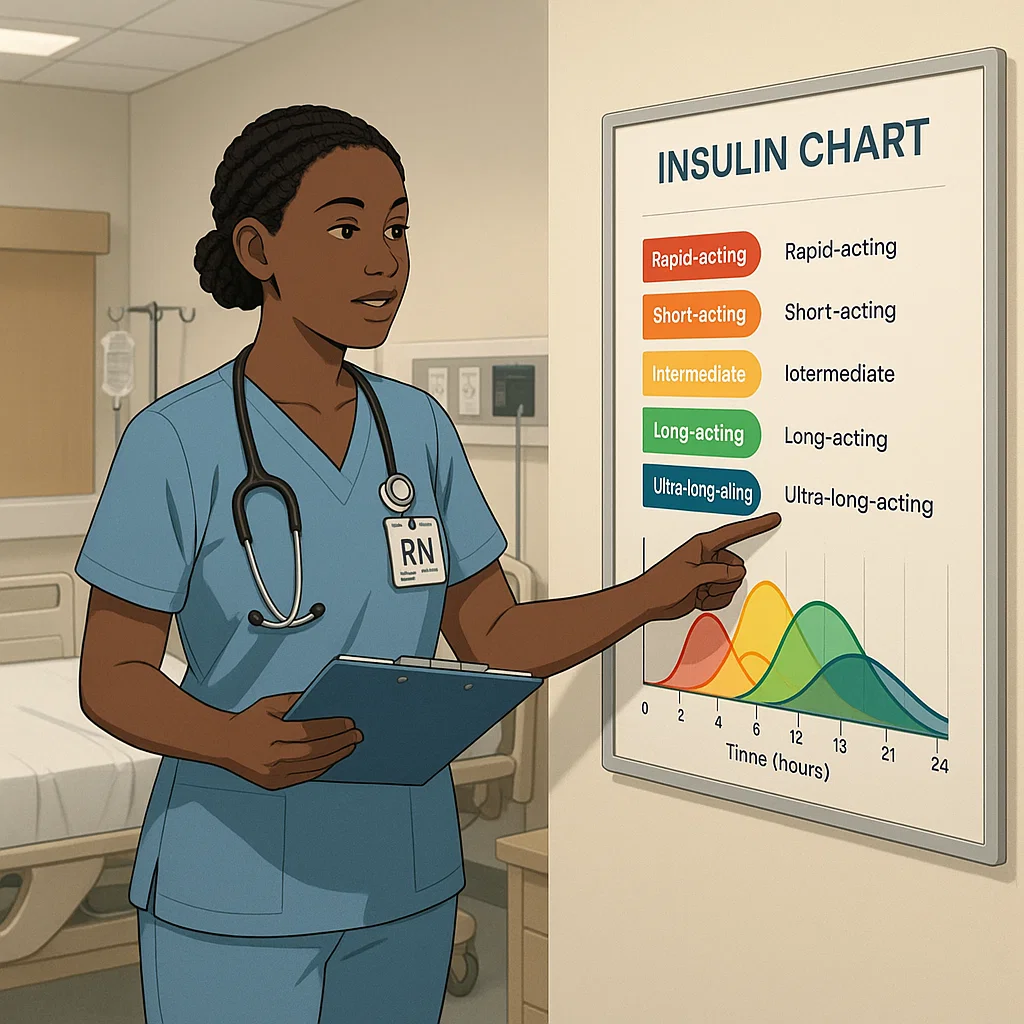
✅ Types of Insulin: Onset, Peak, and Duration
Below is a clear, NCLEX-focused guide. Every nurse should master this table.
🔹 1. Rapid-Acting Insulin
Examples: Lispro (Humalog), Aspart (NovoLog), Glulisine (Apidra)
- Onset: 10–30 minutes
- Peak: 30 minutes–3 hours
- Duration: 3–5 hours
Nursing Tip:
Give immediately before meals. Because onset is fast, the RN nurse must ensure the patient has food available to avoid hypoglycemia.
🔹 2. Short-Acting (Regular) Insulin
Examples: Humulin R, Novolin R
- Onset: 30–60 minutes
- Peak: 2–5 hours
- Duration: 5–8 hours
Nursing Tip:
This is the only insulin given IV during diabetic ketoacidosis (DKA). NCLEX loves this point.
🔹 3. Intermediate-Acting Insulin (NPH)
Examples: Humulin N, Novolin N
- Onset: 1–2 hours
- Peak: 4–12 hours
- Duration: 14–24 hours
Nursing Tip:
Because NPH has a long peak, teach patients to eat snacks to prevent nighttime hypoglycemia.
🔹 4. Long-Acting Insulin
Examples: Glargine (Lantus), Detemir (Levemir)
- Onset: 1–2 hours
- Peak: Minimal or none
- Duration: Up to 24 hours
Nursing Tip:
Never mix long-acting insulin with other insulins. This appears frequently on NCLEX exams.
🔹 5. Ultra-Long-Acting Insulin
Examples: Degludec (Tresiba)
- Onset: 1 hour
- Peak: No significant peak
- Duration: 36–42 hours
Nursing Tip:
Ideal for patients who miss doses because its long duration provides stability.
✅ How Nurses Apply This Information in Practice
To support safe and consistent care, a nurse must:
✅ Coordinate insulin timing with meals
Especially rapid-acting types.
✅ Prevent hypoglycemia
Know peak times to monitor glucose.
✅ Educate patients
Help them understand onset, peak, and duration in simple terms.
✅ Use a nursing bundle or study sheets
These tools reinforce memorization for NCLEX preparation.
✅ NCLEX-Style Memory Tricks
🔹 “15 Minutes Feels Rapid”
Rapid-acting = onset around 15 minutes.
🔹 “Regular insulin is Ready to go IV”
Regular = IV route allowed.
🔹 “NPH is Not Particularly fast or slow”
NPH ≈ intermediate.
🔹 “Lantus = Long and Level”
No peak — stable all day.
These mnemonics help every nursing student strengthen exam readiness.
✅ Conclusion
Insulin therapy is a major NCLEX topic and a key responsibility for every registered nurse. By mastering onset, peak, and duration, both student nurses and experienced clinicians can deliver safer care, prevent complications, and support better patient outcomes. Use this guide along with your nursing bundle to improve memorization and clinical confidence.
FAQ: Insulin Types, Onset, Peak & Duration
Registered nurses preparing for the NCLEX should understand five major insulin types: rapid-acting, short-acting, intermediate-acting, long-acting, and ultra-long-acting. Each category has different onset, peak, and duration times, which directly impact patient monitoring and safe drug administration.
Onset and peak times guide nurses in preventing hypoglycemia, especially around meals. RN nurses must anticipate when insulin activity is strongest to assess symptoms, adjust meals, and intervene quickly if blood glucose drops.
Long-acting insulin, such as glargine (Lantus) or detemir (Levemir), has little to no peak. This makes it ideal for providing a stable 24-hour baseline level of insulin, reducing the risk of hypoglycemia compared to intermediate-acting insulins.