Every nurse knows that understanding wound healing is a crucial part of patient care. Whether you’re preparing for the NCLEX, studying from a nursing bundle, or working as a registered nurse (RN) in a clinical setting, knowing how wounds heal and how to provide the right nursing care can make all the difference in patient recovery.
This guide breaks down the four main stages of wound healing, their clinical signs, and the key nursing interventions every RN nurse should know.
🌿 What Is Wound Healing?
Wound healing is the body’s natural process of repairing damaged tissue after injury. It involves a series of biological steps designed to stop bleeding, prevent infection, and restore skin integrity.
For nursing students and registered nurses, understanding this process is essential to ensure wounds heal properly and complications like infection or delayed healing are avoided.
🩸 Stage 1: Hemostasis — Stopping the Bleeding
Time frame: Immediately after injury
What happens:
When a wound occurs, the body’s first response is to stop the bleeding. Blood vessels constrict, and platelets form a clot to seal the wound. This process prevents further blood loss and creates a temporary barrier against bacteria.
Nursing care tips:
- Apply direct pressure to control bleeding.
- Keep the area clean and dry.
- Document the wound’s size, depth, and cause.
- Educate the patient about avoiding unnecessary movement in the injured area.
🩺 NCLEX tip: Remember that hemostasis involves vasoconstriction and clot formation — a frequent NCLEX question topic.
🌤️ Stage 2: Inflammatory Phase — The Body’s Defense
Time frame: 1 to 5 days after injury
What happens:
During this stage, white blood cells (especially neutrophils and macrophages) move to the wound site to fight infection and clear away debris. This is the body’s immune response to protect and prepare for healing.
Signs you’ll observe:
- Redness
- Warmth
- Swelling
- Mild pain or tenderness
Nursing care tips:
- Monitor for signs of infection (increased redness, pus, fever).
- Keep the wound clean using sterile technique.
- Administer prescribed antibiotics if needed.
- Document wound color, drainage, and odor daily.
💡 Pro tip: These signs are normal in the early phase — but persistent or worsening symptoms may indicate infection, which every RN nurse should report immediately.
🌱 Stage 3: Proliferative Phase — Building New Tissue
Time frame: 5 to 21 days
What happens:
This is when new tissue begins to form. The wound fills with granulation tissue, which looks pink or red and slightly moist. New blood vessels develop, and epithelial cells start covering the wound surface.
Nursing care tips:
- Maintain a moist wound environment — this promotes faster healing.
- Change dressings as ordered using aseptic technique.
- Provide adequate nutrition (especially protein and vitamin C).
- Encourage mobility as tolerated to boost circulation.
📚 NCLEX tip: Moist wound environments support cell growth and reduce scarring — a favorite nursing exam question.
🌼 Stage 4: Maturation (Remodeling) Phase — Strength and Closure
Time frame: 21 days to 1 year (depending on wound severity)
What happens:
In this final phase, collagen strengthens the wound, and scar tissue forms. The area becomes less red and more flexible over time.
Nursing care tips:
- Educate patients about scar care (gentle massage, sunscreen).
- Encourage hydration and balanced nutrition for tissue strength.
- Monitor for keloid formation or abnormal scarring.
- Reassess wound regularly for integrity and flexibility.
🩸 Note for RN nurses: Even though the wound appears closed, full strength may take months to restore. Reinforce this in patient teaching.
⚕️ Factors Affecting Wound Healing
Nurses must be aware of the conditions that delay wound recovery. These include:
- Poor nutrition (low protein, vitamin C, or zinc)
- Diabetes or poor blood circulation
- Smoking and alcohol use
- Infection or repeated trauma to the wound
- Certain medications (e.g., steroids)
✅ Nursing intervention: Assess patient lifestyle, educate on nutrition, and encourage compliance with care plans — these are key NCLEX competencies.
🧠 Nursing Assessment and Documentation
For every registered nurse, accurate wound documentation ensures continuity of care and helps track healing progress. Include:
- Wound size (length, width, depth)
- Color of wound bed (red, yellow, black)
- Drainage amount and type
- Odor, if any
- Condition of surrounding skin
- Patient pain level and tolerance
🩺 NCLEX tip: Always use a consistent wound assessment tool (e.g., the Braden Scale for pressure ulcers).
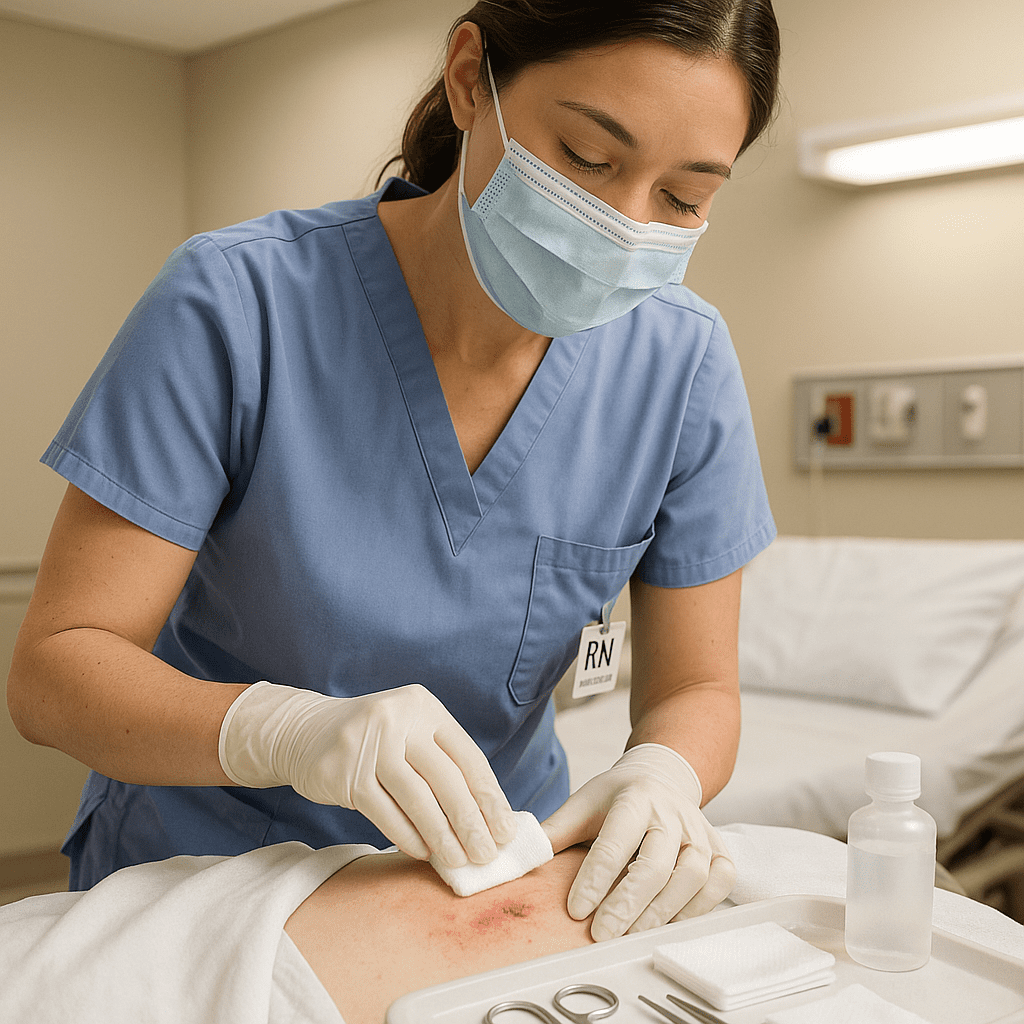
💉 Common Nursing Interventions for Wound Care
- Maintain sterile technique during dressing changes.
- Apply topical medications or ointments as ordered.
- Provide pain management before and after wound care.
- Encourage protein-rich diets and adequate hydration.
- Educate patients about infection prevention and dressing care.
💬 Pro Tip for RN Nurses: Using pre-made nursing bundles with wound care charts and visual guides can simplify patient monitoring and save time in clinical practice.
🏥 Wound Healing and the NCLEX
The NCLEX frequently tests wound healing concepts such as:
- Recognizing wound stages
- Identifying signs of infection
- Prioritizing nursing interventions
- Choosing appropriate dressing types
Example question:
A patient’s wound is red with serous drainage and granulation tissue. Which phase of wound healing is this?
✅ Answer: Proliferative phase.
💡 Final Thoughts
Wound healing is more than just a biological process — it’s a reflection of skilled nursing care and patient education. Whether you’re an aspiring RN nurse studying for the NCLEX or a registered nurse working in a clinical setting, mastering these stages ensures your patients recover safely and efficiently.
🧾 FAQ
Hemostasis, Inflammatory, Proliferative, and Maturation (Remodeling).
By maintaining a moist environment, ensuring good nutrition, preventing infection, and documenting accurately.
Poor circulation, diabetes, malnutrition, smoking, and infection.
Yes, wound care and healing processes are common topics under “Physiological Adaptation.”