Understanding ventricular rhythms is a must for every nurse working in critical care, the ER, or any unit with cardiac monitoring. When the heart’s lower chambers (the ventricles) take over the rhythm, it usually means a serious, life-threatening condition.
In this guide, we’ll break down Ventricular Tachycardia (V-Tach), Ventricular Fibrillation (V-Fib), and Asystole — how to identify them on an EKG, common causes, patient signs, and what you must do quickly to save a life.
❤️ What Are Ventricular Rhythms?
Normally, the heart’s electrical signal starts in the atria (upper chambers) and flows down to the ventricles. Sometimes, however, the ventricles fire on their own — and they are bad at it. This can cause extremely fast, disorganized, or absent heartbeats.
Key point: When the ventricles run the show, your patient is often in danger of cardiac arrest!
💓 1️⃣ Ventricular Tachycardia (V-Tach)
🔍 What is V-Tach?
V-Tach happens when the ventricles beat fast — usually 100–250 beats per minute — and override the normal pacemaker.
It can be:
- Stable V-Tach: Patient has a pulse and some blood pressure.
- Unstable V-Tach: Patient has a pulse but is weak, dizzy, or about to collapse.
- Pulseless V-Tach: No pulse = cardiac arrest.
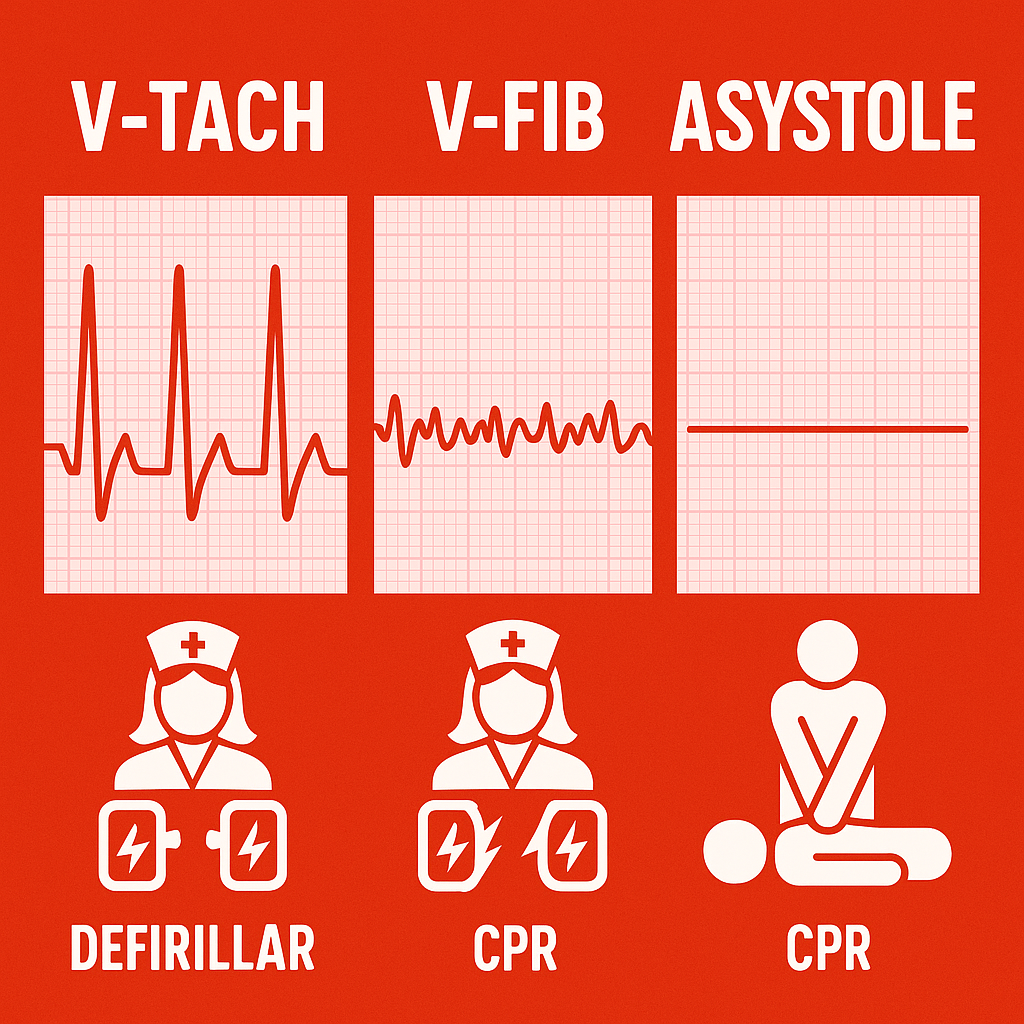
🩺 How to Recognize V-Tach
On an EKG:
- Wide, tall, bizarre QRS complexes.
- No clear P waves.
- Regular rhythm.
It looks like big mountains or tombstones in a row.
⚡ Causes of V-Tach
- Heart attack or scarring after an MI.
- Electrolyte imbalance (low potassium or magnesium).
- Drug toxicity (like digoxin).
- Heart failure.
🚑 Nursing Actions for V-Tach
- Check the patient! Confirm if there’s a pulse.
- If pulseless: Start CPR and defibrillate immediately.
- If with pulse but unstable: Prepare for synchronized cardioversion.
- Give meds: Amiodarone, lidocaine, or magnesium as ordered.
- Treat underlying causes: Correct electrolytes, review medications.
💙 2️⃣ Ventricular Fibrillation (V-Fib)
🔍 What is V-Fib?
V-Fib is chaotic, disorganized electrical activity in the ventricles. They quiver instead of contracting — so NO blood gets pumped. This is cardiac arrest!
🩺 How to Recognize V-Fib
On an EKG:
- No identifiable QRS complexes.
- No P waves.
- Wavy, irregular, chaotic line — no pattern.
Think “scribble line of death.”
⚡ Causes of V-Fib
- Acute MI.
- Severe electrolyte imbalance.
- Electric shock.
- Advanced cardiac disease.
🚑 Nursing Actions for V-Fib
- Check responsiveness: Patient is unresponsive and pulseless.
- Call a Code Blue immediately!
- Start high-quality CPR immediately.
- Defibrillate as soon as possible: Shock, CPR, shock.
- Administer meds: Epinephrine and amiodarone as ordered.
- Keep monitoring: Repeat shocks and drugs per ACLS.
🖤 3️⃣ Asystole
🔍 What is Asystole?
Asystole is flatline — the heart has no electrical activity. It’s the end stage of cardiac arrest and very hard to reverse.
🩺 How to Recognize Asystole
On an EKG:
- A flat line.
- No P waves, no QRS, nothing.
⚠️ Be careful: check other leads to confirm. Sometimes a loose lead looks like asystole but isn’t!
⚡ Causes of Asystole
- Untreated V-Fib or severe cardiac damage.
- Massive MI.
- Severe hypoxia.
- Advanced end-stage disease.
🚑 Nursing Actions for Asystole
- Check the patient! Confirm no pulse.
- Start high-quality CPR immediately.
- Do NOT defibrillate: Shocking a flatline won’t help.
- Give meds: Epinephrine every 3–5 minutes.
- Find and treat reversible causes: 5 H’s and 5 T’s (hypoxia, hypovolemia, H+ (acidosis), hypo/hyperkalemia, hypothermia, toxins, tamponade, tension pneumothorax, thrombosis (MI/PE), trauma).
📊 Key EKG Differences
| Rhythm | EKG Look | Pulse? | Shock? | Main Action |
|---|---|---|---|---|
| V-Tach | Wide QRS, fast | Maybe | Yes (if unstable/pulseless) | Cardioversion or defibrillation |
| V-Fib | Wavy, chaotic | No | Yes | Defibrillate ASAP |
| Asystole | Flat line | No | No | CPR + Epi only |
⚕️ Why Nurses Must Master These Rhythms
Ventricular rhythms can kill within minutes if not treated quickly. As a nurse:
✅ Recognize them immediately.
✅ Confirm with patient assessment.
✅ Call for help, start CPR, and use the defibrillator properly.
✅ Follow ACLS steps and communicate clearly with the team.
💡 Quick Nurse Tips
- Trust your eyes: Learn to read EKG strips fast — practice daily.
- Never just trust the monitor: Check the patient.
- Stay calm: In codes, calm nurses are lifesavers.
- Document well: Record times of pulses, shocks, meds.
- Debrief after a code: Learn what went well and what could improve.
🏥 Conclusion
V-Tach, V-Fib, and Asystole are the scariest rhythms you’ll face — but you can handle them. Know how to spot them, stay ready to act, and work with your team. Remember: your quick action can mean the difference between life and death.
Keep practicing — lives depend on it!