Targeted Temperature Management (TTM) is a critical post–cardiac arrest intervention that significantly impacts neurological outcomes and survival. For every nurse, especially the ICU registered nurse (RN nurse), understanding TTM is essential for delivering evidence-based nursing care. Because post–cardiac arrest management is heavily tested on the NCLEX, mastering TTM concepts is vital both for exam success and bedside competency.
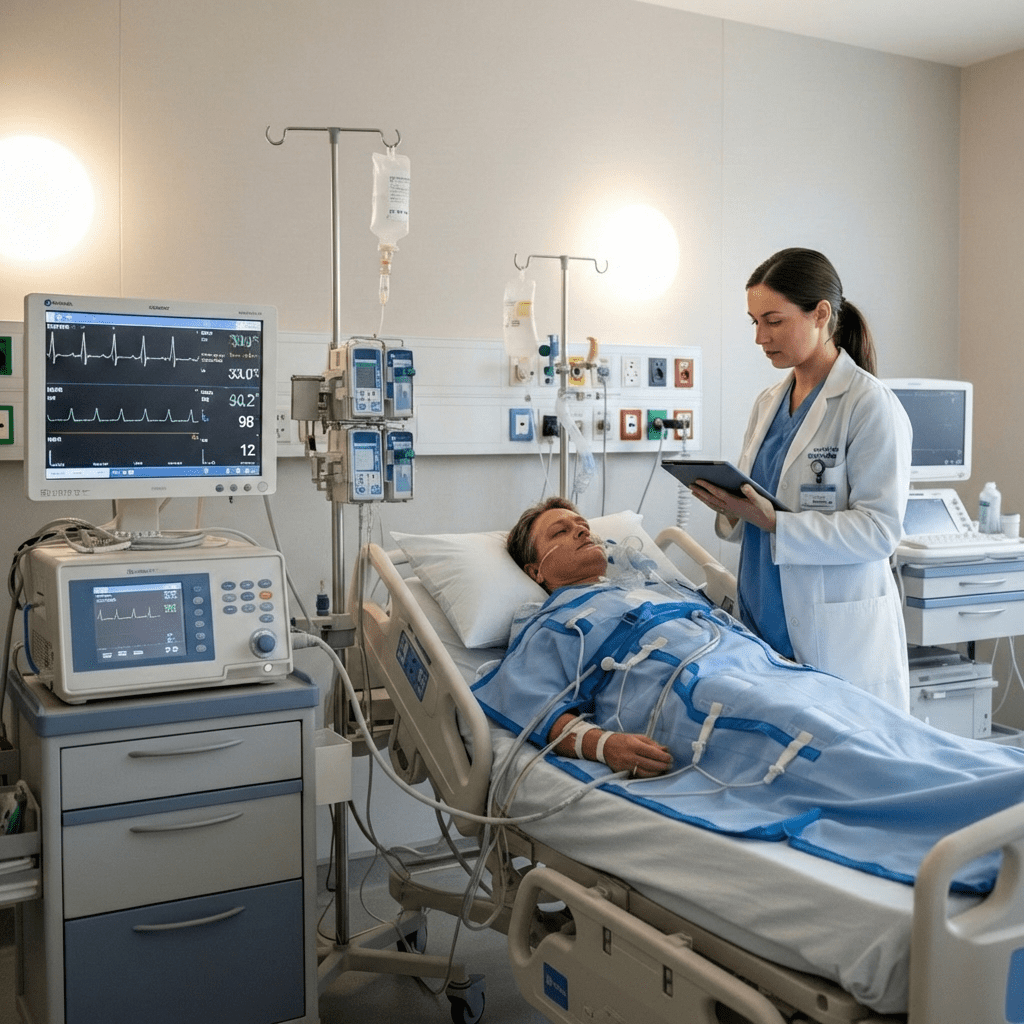
In modern critical care practice, TTM is often incorporated into a structured post–cardiac arrest nursing bundle, ensuring standardized, high-quality care that improves patient outcomes.
What Is Targeted Temperature Management?
Targeted Temperature Management is a controlled therapeutic intervention that lowers and maintains a patient’s core body temperature after return of spontaneous circulation (ROSC) following cardiac arrest.
The goal:
Reduce cerebral metabolic demand and minimize hypoxic brain injury.
TTM is primarily used in comatose adult patients after:
- Out-of-hospital cardiac arrest
- In-hospital cardiac arrest
- Ventricular fibrillation (VF)
- Pulseless ventricular tachycardia (VT)
- Selected non-shockable rhythms
For the RN nurse in critical care, TTM is a time-sensitive, protocol-driven intervention requiring precise monitoring.
Why Temperature Control Matters After Cardiac Arrest
After cardiac arrest, the brain experiences global ischemia. Even after ROSC, reperfusion injury can worsen neuronal damage.
Without temperature control:
- Cerebral edema may worsen
- Inflammatory cascades increase
- Neurological outcomes decline
By reducing body temperature, TTM slows metabolic processes and protects brain tissue.
This pathophysiology is commonly tested on the NCLEX under post-resuscitation care.
Target Temperature Goals
Current guidelines typically recommend maintaining a temperature between:
32°C and 36°C (89.6°F–96.8°F)
The exact target depends on institutional protocols. Once selected, the temperature must be maintained consistently for at least 24 hours.
For the registered nurse, strict adherence to protocol is critical.
Phases of Targeted Temperature Management
TTM occurs in three structured phases. Understanding these phases is essential in both clinical nursing practice and NCLEX scenarios.
1. Induction Phase
Goal: Rapidly achieve target temperature.
Methods include:
- Surface cooling blankets
- Ice packs
- Cooling pads
- Intravascular cooling devices
- Cold IV fluids (depending on protocol)
Nursing priorities during induction:
- Continuous core temperature monitoring
- Sedation administration
- Prevention of shivering
- Hemodynamic stabilization
Shivering increases oxygen demand, which counteracts TTM benefits. Therefore, the RN nurse must recognize early signs of shivering and intervene promptly.
2. Maintenance Phase
Goal: Maintain consistent target temperature for 24 hours.
Nursing responsibilities include:
- Continuous cardiac monitoring
- Frequent neurological assessment
- Strict intake and output measurement
- Electrolyte monitoring
- Glucose control
- Prevention of skin breakdown
TTM affects multiple body systems. The registered nurse must anticipate complications rather than react to them.
3. Rewarming Phase
Goal: Slowly return patient to normothermia.
Rewarming must be gradual (typically 0.25–0.5°C per hour).
Rapid rewarming can cause:
- Hypotension
- Electrolyte shifts
- Increased intracranial pressure
- Arrhythmias
During this phase, vigilant nursing assessment is essential.
Common Complications of TTM
Understanding complications is essential for both bedside practice and NCLEX preparation.
1. Cardiac Arrhythmias
Bradycardia is common and often expected during cooling.
2. Electrolyte Imbalances
- Hypokalemia during cooling
- Hyperkalemia during rewarming
3. Coagulopathy
Hypothermia impairs clotting mechanisms.
4. Hyperglycemia
Stress response and insulin resistance occur.
5. Infection Risk
Hypothermia suppresses immune response.
The RN nurse must anticipate these complications and intervene early.
Sedation and Paralysis in TTM
Because shivering increases metabolic demand, patients undergoing TTM often require:
- Sedation
- Analgesia
- Neuromuscular blockade (if shivering persists)
Nursing implications include:
- Train-of-four monitoring
- Ensuring adequate sedation before paralysis
- Preventing awareness
These sedation principles are frequently tested on the NCLEX in critical care questions.
Hemodynamic Monitoring During TTM
TTM can impact:
- Blood pressure
- Heart rate
- Cardiac output
Vasopressors may be required. Continuous monitoring by the critical care nurse is essential.
TTM integrates closely with other ICU nursing bundles such as:
- Sepsis bundle
- Ventilator bundle
- Hemodynamic optimization protocols
Comprehensive nursing care ensures improved neurological outcomes.
Nursing Assessment Priorities
During TTM, the registered nurse should focus on:
- Core temperature (esophageal, bladder, or intravascular probe)
- Cardiac rhythm
- Blood pressure trends
- Urine output
- Electrolyte levels
- Blood glucose
- Skin integrity
- Neurological status
Frequent documentation is essential for both patient safety and interdisciplinary communication.
Ethical Considerations and Family Education
Family members may be distressed when they see a cooled, sedated, unresponsive patient.
The nurse plays a key role in:
- Explaining the purpose of TTM
- Clarifying sedation use
- Providing emotional support
- Setting realistic expectations
Compassionate communication is a core component of professional nursing practice.
TTM and the NCLEX
On the NCLEX, questions about post–cardiac arrest care often test:
- Priority interventions
- Prevention of shivering
- Slow rewarming principles
- Monitoring for electrolyte shifts
- Expected bradycardia during hypothermia
The safest answer often includes continuous monitoring and gradual rewarming rather than rapid correction.
Incorporating TTM into a Nursing Bundle
A structured post–cardiac arrest nursing bundle may include:
- Airway and oxygenation optimization
- Hemodynamic stabilization
- Targeted temperature management
- Glucose control
- Seizure monitoring
- Neurological assessment
For the RN nurse, understanding how TTM fits into a broader bundle improves both patient outcomes and professional confidence.
High-Yield NCLEX Summary
- TTM is used after ROSC in comatose patients
- Target temperature: 32–36°C
- Cooling lasts 24 hours
- Rewarm slowly
- Monitor electrolytes carefully
- Bradycardia during cooling may be expected
- Prevent shivering
Final Thoughts
Targeted Temperature Management is a cornerstone of modern post–cardiac arrest care. For every nurse working in emergency or critical care settings, mastering TTM enhances clinical competence and improves neurological outcomes.
Because post–resuscitation management is heavily emphasized on the NCLEX, a solid understanding of TTM principles is essential for nursing students and registered nurses alike. When incorporated into a structured nursing bundle, TTM becomes a powerful, life-preserving intervention guided by evidence-based nursing practice.