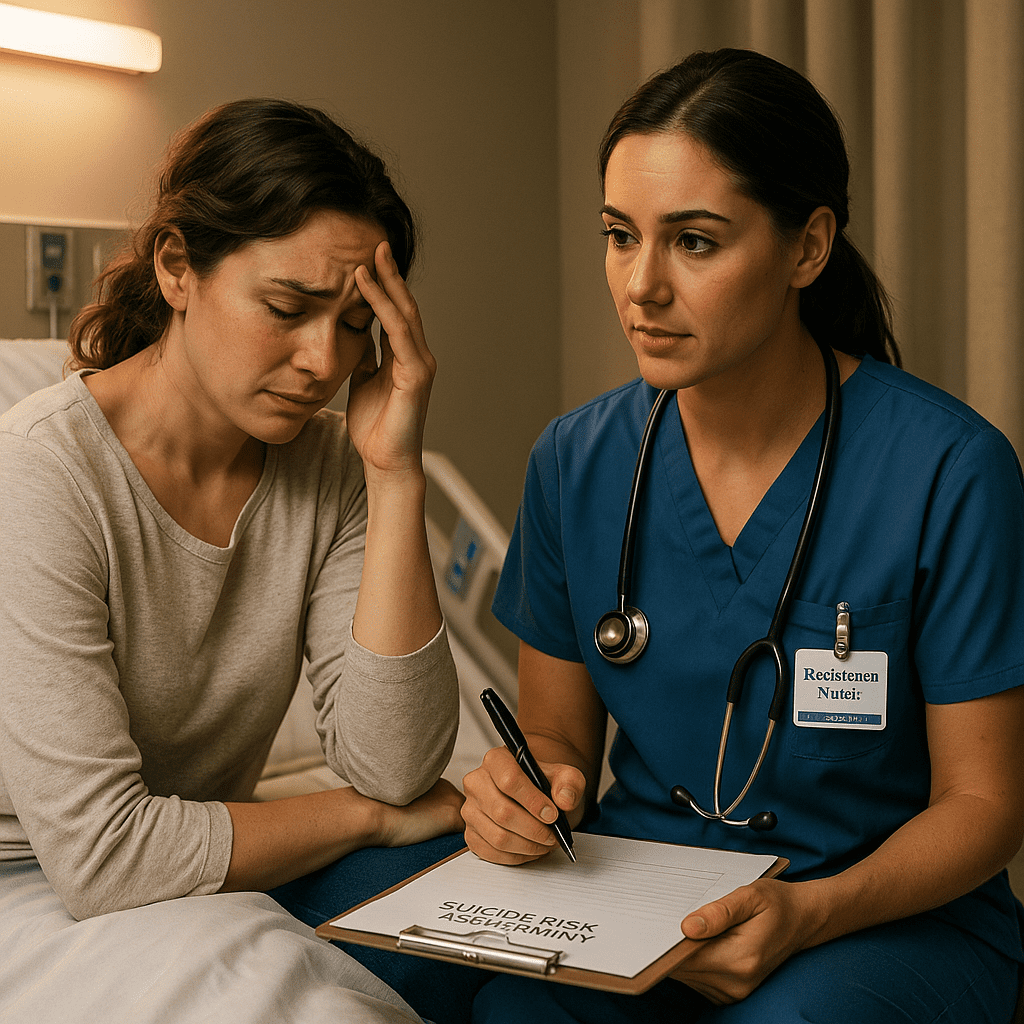
In the world of nursing, few conversations are more delicate — or more important — than assessing a patient’s risk for suicide.
Whether you’re a registered nurse, an RN nurse in mental health, or a student preparing for the NCLEX, understanding how to ask the right questions can literally save a life.
This guide breaks down what every nurse must know about suicide risk assessment, how to recognize warning signs, and how to respond effectively.
💡 Why Suicide Risk Assessment Matters
Suicide prevention starts with early recognition.
Many patients who are at risk show signs before attempting suicide — and the nurse is often the first to notice.
In both hospital and community settings, the registered nurse plays a key role in identifying verbal, emotional, and behavioral cues that signal danger.
🚨 Warning Signs Nurses Must Recognize
Before asking questions, every nurse should be alert for these warning signs:
- Expressing hopelessness or saying things like “I can’t go on.”
- Withdrawal from friends, family, or social activities.
- Sudden mood improvement after a period of depression (this can signal decision to act).
- Giving away personal items or saying goodbye.
- History of suicide attempts or self-harm.
- Access to firearms, medications, or other means.
Recognizing these cues early is part of safe nursing practice and often appears on NCLEX questions related to mental health nursing.
🩺 What Nurses Must Ask During Suicide Risk Assessment
When assessing suicide risk, the nurse should remain calm, compassionate, and nonjudgmental.
Here are the essential questions every RN nurse should ask:
1. “Are you thinking about hurting yourself?”
This is the most direct and vital question.
It helps determine presence of suicidal thoughts (ideation). Asking directly does not plant the idea — it shows concern and allows open communication.
2. “Do you have a plan?”
If the patient says yes, the nurse must find out how specific the plan is.
A detailed plan (time, place, method) = higher risk.
3. “Do you have access to the means?”
If a patient mentions using a gun, pills, or another method, assess whether they have access to those items.
If yes, remove them immediately or ensure supervision and safety.
4. “Have you tried to harm yourself before?”
A history of attempts increases risk dramatically.
The registered nurse should document past incidents and communicate them to the healthcare team.
5. “What has stopped you from acting on your thoughts?”
This question helps explore protective factors — like family, faith, or hope for the future.
Nurses can use these to strengthen the patient’s support system.
🧩 Nursing Interventions for Suicidal Patients
Once risk is identified, nursing care focuses on safety and support:
- Stay with the patient — never leave them alone if high risk.
- Remove sharp objects, cords, and medications.
- Document findings and report immediately to the provider.
- Provide emotional support and build trust.
- Encourage participation in therapy and coping strategies.
In nursing bundles and NCLEX mental health prep, this scenario is a common topic under Psychosocial Integrity — knowing priority actions saves both points and lives.
📋 Nursing Priorities (NCLEX Focus)
For the NCLEX, remember the ABCs + Safety rule:
- Assess for suicidal thoughts.
- Ensure safety (remove means, constant observation).
- Communicate findings to the mental health team.
- Support with empathy, not judgment.
If the question asks what to do first — the correct answer is “Assess the level of suicide risk.”
🧠 Example NCLEX Tip
Question: A patient states, “I just want to go to sleep and never wake up.” What is the nurse’s priority action?
✅ Answer: Ask directly, “Are you thinking about hurting yourself?”
💡 Rationale: Always assess suicidal ideation before taking further steps. Avoid ignoring or minimizing the statement.
💬 Therapeutic Communication Phrases
When talking to a suicidal patient, avoid judgmental or minimizing statements like:
❌ “You have so much to live for.”
❌ “You wouldn’t really do that, would you?”
Instead, use therapeutic phrases:
✅ “Tell me more about how you’re feeling.”
✅ “You seem very hopeless right now. I’m here to help you.”
✅ “I’m glad you told me — let’s find a way to keep you safe.”
These are nursing communication skills tested on the NCLEX and taught in most mental health nursing bundles.
🧾 Key Takeaways for Nurses
- Suicide assessment starts with asking direct, compassionate questions.
- Never ignore verbal or behavioral warning signs.
- Safety comes first — ensure supervision and remove dangerous objects.
- Document and report all findings promptly.
- Build trust with therapeutic communication.
Whether you’re a student nurse preparing for the NCLEX or a registered nurse on the front lines, mastering suicide risk assessment is a vital skill in every area of nursing practice.
🩺 Final Thought
Being a nurse means being more than a caregiver — it means being a lifeline.
The questions you ask, the compassion you show, and the safety you provide can make the difference between life and loss.
Keep learning, keep listening, and always trust your nursing instincts.
🧠 FAQs – Suicide Risk Assessment for Nurses
The first step for any registered nurse (RN) is to establish a safe and private environment for the patient. Building trust through therapeutic communication helps the patient feel comfortable sharing thoughts of self-harm. According to NCLEX nursing guidelines, you must directly ask about suicidal thoughts rather than avoid the topic — this shows care and professionalism.
When conducting a suicide risk assessment, nurses should ask:
“Are you thinking about hurting yourself?”
“Do you have a plan to harm yourself?”
“Do you have access to means, such as medication or weapons?”
These questions help the RN nurse determine intent, plan, and lethality, which are vital in deciding whether the patient needs immediate intervention or hospitalization.
Nursing students and registered nurses should recognize these high-risk signs:
Expressing hopelessness or saying “I have no reason to live.”
Giving away personal belongings.
Withdrawing from family and social life.
Sudden mood improvement after a long depression (a red flag before suicide).
If a patient confirms suicidal thoughts, the nurse must never leave the patient alone. Follow hospital protocols:
Notify the charge nurse or provider immediately.
Remove any potential means of self-harm from the area.
Initiate constant observation or 1:1 supervision if required.
These steps are crucial for patient safety and are highly testable topics on the NCLEX.
Documentation is a legal and clinical responsibility. The RN nurse should record:
The exact patient statements about suicidal thoughts.
Assessment findings (plan, intent, means).
Interventions and who was notified.
Patient’s response to interventions.
Accurate, objective documentation protects both patient safety and the nurse’s practice.