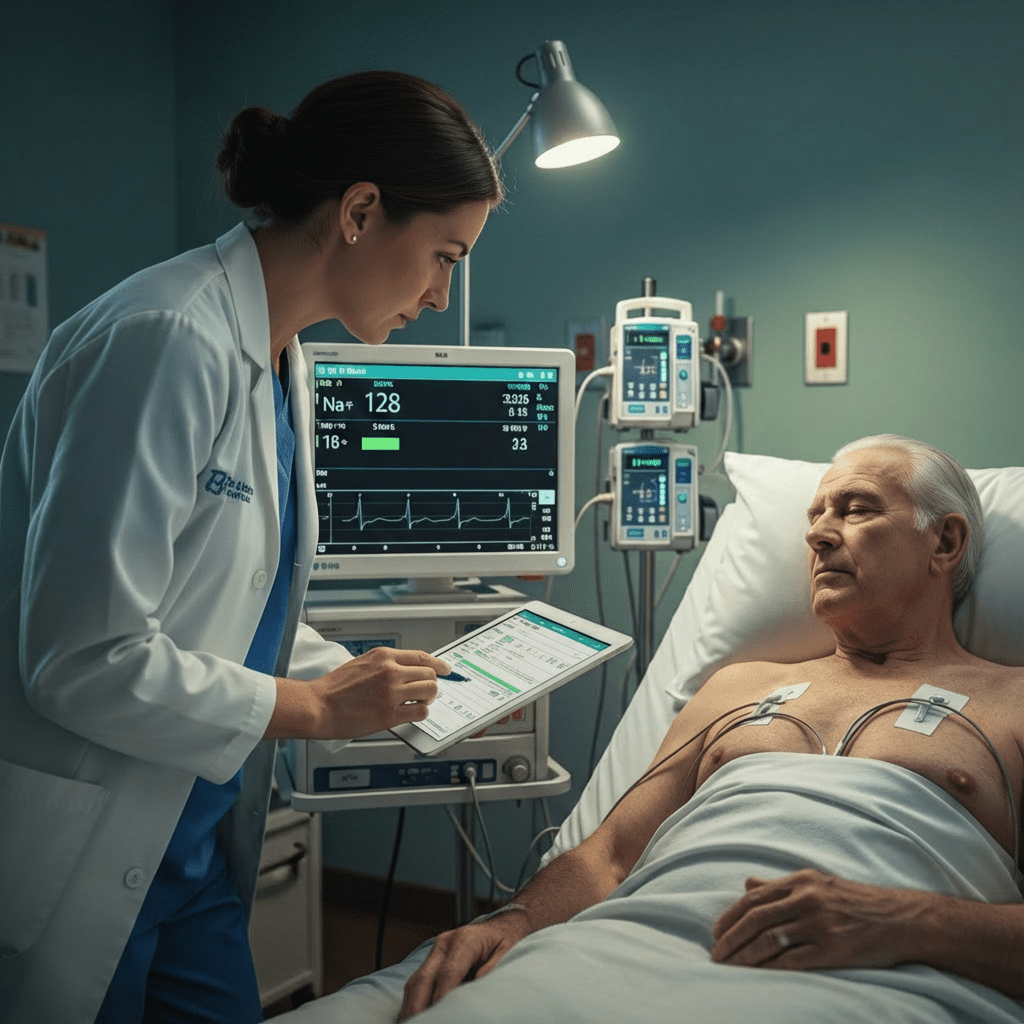
Sodium disorders are extremely common in patients with heart failure, and every nurse, registered nurse, and RN nurse must understand how to assess, monitor, and intervene. Whether you’re preparing for the NCLEX, updating your nursing knowledge, or using a nursing bundle to study fluid and electrolyte imbalances, this guide will help simplify everything you need to know.
🔍 Why Sodium Disorders Occur in Heart Failure
Heart failure affects the kidneys and hormonal systems responsible for sodium and water balance. As cardiac output decreases:
- The body activates RAAS (renin–angiotensin–aldosterone system)
- ADH (antidiuretic hormone) increases
- The kidneys retain water
- Sodium becomes diluted
This leads to dilutional hyponatremia, the most common sodium disorder in heart failure patients.
🧂 1. Hyponatremia in Heart Failure
What It Is
Hyponatremia = serum sodium < 135 mEq/L.
Why It Happens
- Water retention > sodium retention
- Excessive diuretics
- SIADH triggered by severe heart failure
Nursing Assessment
A registered nurse should monitor for:
- Confusion or headache
- Nausea and vomiting
- Muscle cramps
- Seizures (severe)
- Low serum sodium
- Low serum osmolality
Nursing Interventions
- Fluid restriction (most common intervention)
- Monitor daily weights
- Strict I&O
- Monitor neuro status
- Evaluate diuretic dosing
- Administer hypertonic saline (3%) if severe and symptomatic
- Educate patient on limiting fluid intake
NCLEX Tip
Hyponatremia in HF is almost always dilutional, NOT a sodium-loss problem.
🧂 2. Hypernatremia in Heart Failure
Much less common but dangerous.
Why It Happens
- Excess diuresis
- Lack of free water intake
- Tube feedings without adequate water flushes
- Overuse of hypertonic fluids
Nursing Assessment
- Thirst
- Dry mucous membranes
- Decreased skin turgor
- Agitation or restlessness
- Tachycardia
- High serum sodium (>145 mEq/L)
Nursing Interventions
- Replace free water slowly
- Stop hypertonic sodium products
- Monitor neuro status closely
- Evaluate medication list
- Ensure water flushes for tube-fed patients
NCLEX Warning
Correct sodium slowly to prevent cerebral edema.
🧠 Clinical Priority for Nurses
Sodium disorders can quickly turn into life-threatening emergencies, so the RN nurse must:
- Monitor labs daily
- Reassess mental status
- Evaluate response to diuretics
- Communicate with the provider about rapid sodium changes
- Document symptoms and interventions clearly
🧪 Evidence-Based Nursing Interventions for NCLEX
| Disorder | Expected Labs | Priority Nursing Action |
|---|---|---|
| Hyponatremia | Na <135 | Fluid restriction |
| Hypernatremia | Na >145 | Free water replacement |
| Severe symptoms | Altered LOC, seizures | Administer hypertonic saline (carefully) |