Sedation and pain management are vital components of critical care nursing. In the intensive care unit (ICU), patients often experience pain, anxiety, and discomfort due to invasive procedures, mechanical ventilation, or serious illness. For every registered nurse (RN), mastering sedation protocols and pain control strategies is essential for both safe patient care and NCLEX success.
🩺 Understanding Sedation in the ICU
Sedation in the ICU helps reduce anxiety, agitation, and pain while improving patient-ventilator synchrony. It also facilitates procedures such as intubation or central line placement. However, over-sedation can lead to complications like delirium, hypotension, or prolonged mechanical ventilation—making nursing assessment and titration critical.
Common Sedatives Used in the ICU:
- Propofol: Rapid onset, short duration; monitor for hypotension and respiratory depression.
- Midazolam (Versed): Benzodiazepine used for short-term sedation; monitor for confusion and accumulation in renal impairment.
- Dexmedetomidine (Precedex): Provides sedation without significant respiratory depression; useful for weaning from mechanical ventilation.
Nursing Responsibilities:
- Continuously monitor sedation depth using scales (e.g., RASS or Ramsay Sedation Scale).
- Reassess need for sedation regularly.
- Watch for hypotension, bradycardia, or respiratory changes.
- Document medication titration and patient response accurately in the nursing bundle.
💊 Pain Control Strategies in the ICU
Pain is one of the most underrecognized symptoms in critically ill patients. Registered nurses must proactively assess and manage it using evidence-based interventions.
Common Analgesics:
- Opioids (Morphine, Fentanyl, Hydromorphone): Mainstay for severe pain; monitor for respiratory depression.
- Acetaminophen: Used for mild pain or fever; watch for hepatotoxicity.
- NSAIDs: Effective for musculoskeletal pain; monitor renal function and gastrointestinal side effects.
Non-Pharmacologic Interventions:
- Adjusting patient positioning and comfort measures.
- Providing a calm environment to reduce anxiety.
- Using relaxation techniques or guided imagery.
Combining pharmacologic and non-pharmacologic methods ensures comprehensive nursing care.
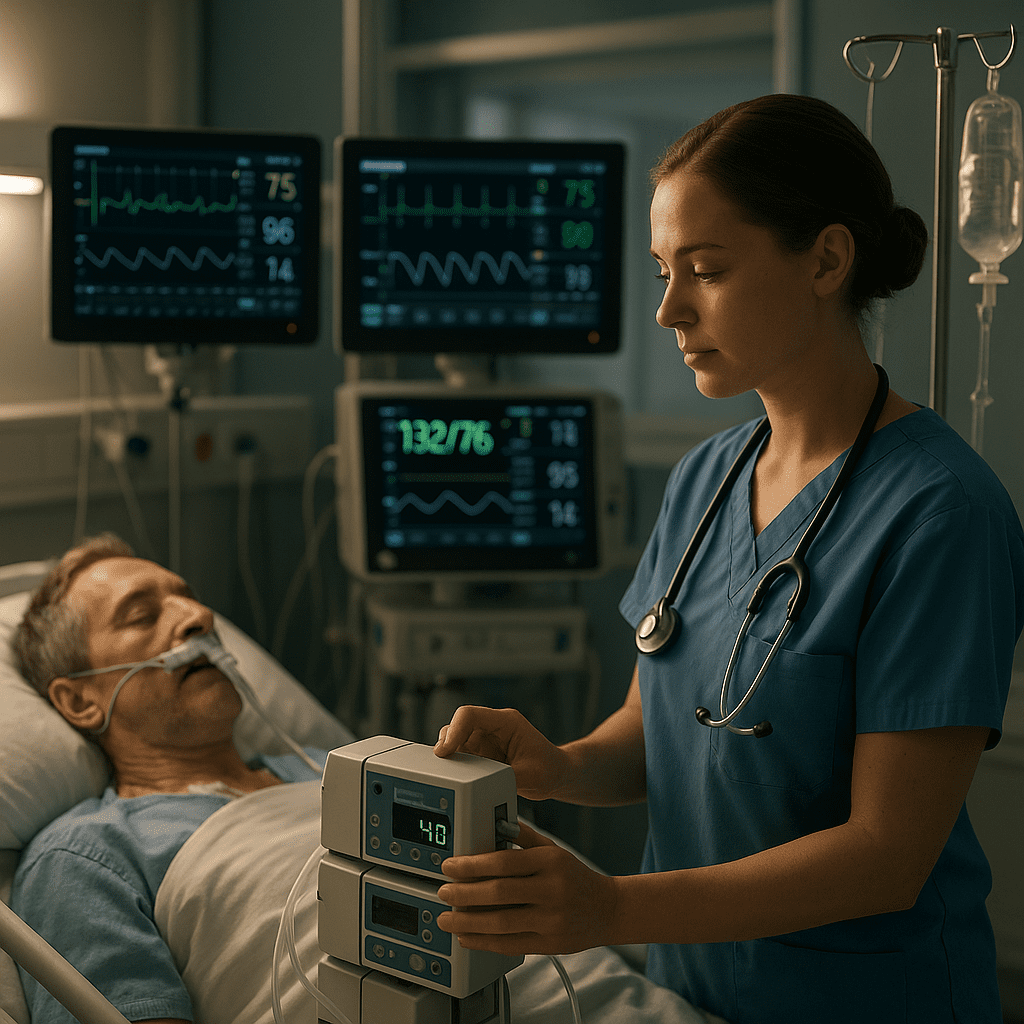
⚕️ Nursing Assessment and Monitoring
Effective sedation and pain control require ongoing assessment. The RN nurse must evaluate:
- Pain levels: Use scales such as the Critical-Care Pain Observation Tool (CPOT).
- Sedation depth: Aim for light sedation unless otherwise indicated.
- Vital signs: Monitor for changes in blood pressure, respiratory rate, and oxygen saturation.
- Neurological status: Evaluate responsiveness and signs of delirium.
Timely documentation and collaboration with the ICU team are part of essential nursing responsibilities.
🧠 NCLEX Tips for Nurses
For NCLEX questions, remember these key principles:
- Always assess pain before administering sedatives.
- Sedation should never mask unrelieved pain.
- Monitor for respiratory depression with opioids or sedatives.
- Use reversal agents appropriately (e.g., naloxone for opioids, flumazenil for benzodiazepines).
Understanding these concepts ensures patient safety and supports success in NCLEX pharmacology and critical care scenarios.
👩⚕️ Role of the Registered Nurse in the ICU
The registered nurse plays a central role in coordinating sedation and pain management. Responsibilities include:
- Assessing pain and sedation needs.
- Administering and titrating medications per protocol.
- Monitoring patient responses and communicating changes to physicians.
- Educating families about the patient’s sedation plan.
These tasks align with professional nursing standards and are reinforced through structured nursing bundles used in ICU settings.
🧩 Key Takeaway for Nurses
Effective sedation and pain control are cornerstones of ICU nursing care. For every RN nurse, maintaining vigilance, assessing accurately, and intervening appropriately can make the difference between recovery and complication. Whether preparing for the NCLEX or working in critical care, understanding these principles empowers nurses to deliver safe, compassionate, and evidence-based care.
💬 FAQ: Sedation and Pain Control in the ICU
The goal of sedation in the ICU is to keep critically ill patients calm, comfortable, and safe while allowing for necessary treatments like mechanical ventilation. Nurses assess the patient’s sedation level frequently to ensure the right balance between comfort and responsiveness.
Even when a patient is sedated, nurses use validated pain scales such as the Behavioral Pain Scale (BPS) or the Critical-Care Pain Observation Tool (CPOT). These help measure non-verbal signs like facial expression, muscle tension, or ventilator synchrony.
Common sedatives include propofol, midazolam, and dexmedetomidine. For pain control, fentanyl or morphine may be used. RNs must monitor for respiratory depression, hypotension, and changes in mental status.
The registered nurse (RN) plays a vital role by:
Monitoring sedation depth and pain levels
Adjusting medication per protocol
Preventing complications like delirium or oversedation
Educating the care team and patient’s family about sedation goals