Refeeding syndrome is one of the most dangerous — and often overlooked — electrolyte emergencies in clinical practice. For any nurse, especially a critical care registered nurse (RN nurse), recognizing early signs of refeeding syndrome can prevent cardiac arrest, respiratory failure, and sudden death. Because it involves rapid electrolyte shifts, it is a high-yield concept for the NCLEX and essential knowledge in advanced nursing care.
Refeeding syndrome is not caused by starvation alone — it is triggered when nutrition is reintroduced too quickly.
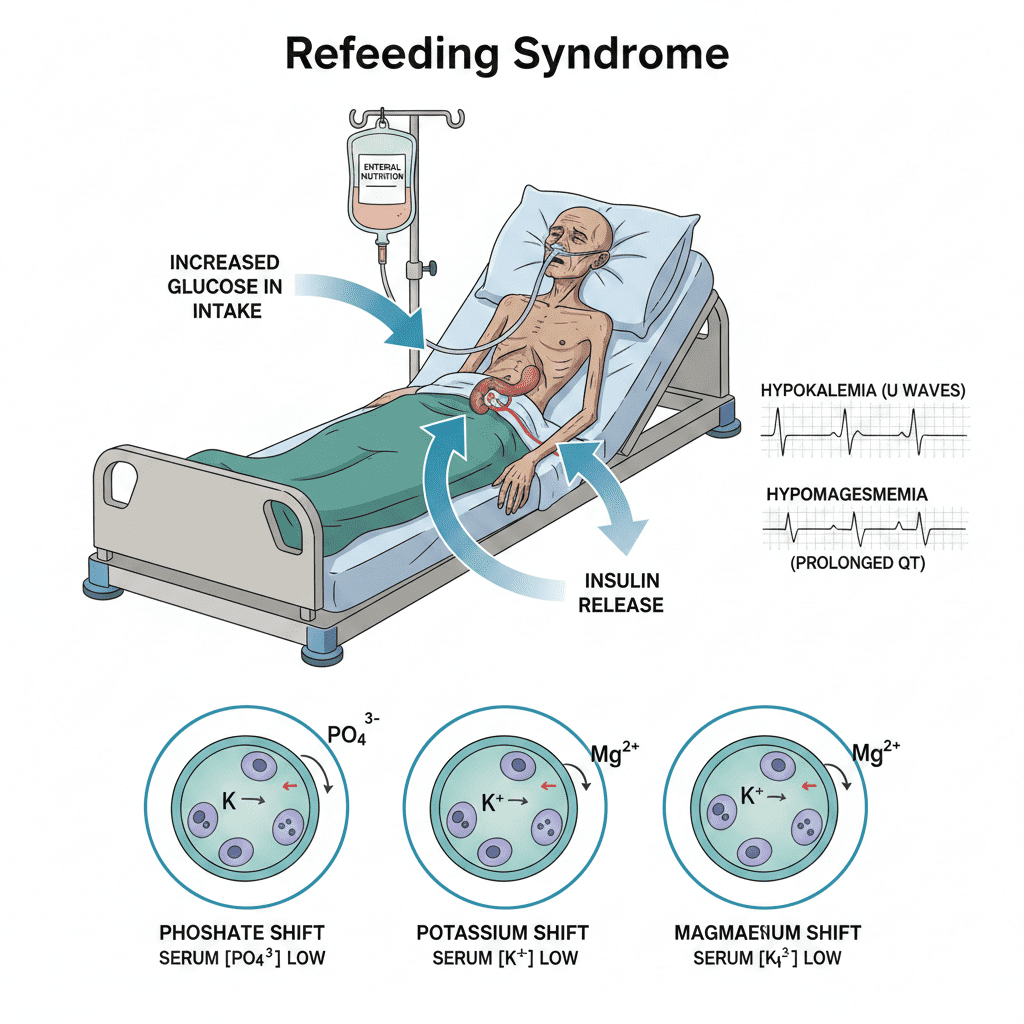
Refeeding syndrome occurs when rapid carbohydrate intake causes insulin release, driving phosphate, potassium, and magnesium into cells — leading to sudden electrolyte collapse.
What Is Refeeding Syndrome?
Refeeding syndrome is a metabolic disturbance that occurs when a malnourished patient begins receiving nutrition again (oral, enteral, or parenteral).
The hallmark feature:
- Severe hypophosphatemia
But it also includes:
- Hypokalemia
- Hypomagnesemia
- Thiamine deficiency
- Fluid shifts
- Glucose instability
For the RN nurse, understanding the cellular mechanism is crucial.
The Cellular Mechanism Behind Refeeding Syndrome
During starvation:
- Insulin levels are low
- The body shifts to fat and protein metabolism
- Intracellular electrolytes become depleted
- Serum levels may appear “normal”
When carbohydrates are reintroduced:
1️⃣ Blood glucose rises
2️⃣ Insulin secretion increases
3️⃣ Glucose enters cells
4️⃣ Phosphate, potassium, and magnesium shift into cells
Serum electrolyte levels suddenly drop.
This shift creates electrical and metabolic instability — a core NCLEX concept.
Why Phosphate Is the Most Dangerous Drop
Phosphate is essential for:
- ATP production
- Oxygen delivery (2,3-DPG in RBCs)
- Muscle contraction
- Cardiac function
Severe hypophosphatemia can cause:
- Respiratory failure (weak diaphragm)
- Decreased cardiac contractility
- Arrhythmias
- Seizures
The registered nurse must monitor phosphate levels closely when initiating nutrition in malnourished patients.
Patients at High Risk
The nurse should suspect refeeding syndrome in patients with:
- Eating disorders
- Chronic alcoholism
- Prolonged NPO status
- Cancer cachexia
- Bariatric surgery complications
- Uncontrolled diabetes
- Severe malnutrition
This risk assessment is commonly tested on the NCLEX.
Clinical Signs and Symptoms
Electrolyte collapse may present as:
- Weakness
- Edema
- Tachycardia
- Arrhythmias
- Confusion
- Seizures
- Respiratory distress
ECG changes may reflect:
- Hypokalemia (U waves)
- Hypomagnesemia (prolonged QT)
The RN nurse must correlate labs with telemetry findings.
The Role of Insulin in Electrolyte Shifts
Insulin stimulates:
- Sodium-potassium ATPase
- Cellular uptake of glucose
- Movement of potassium into cells
- Movement of phosphate into cells
This rapid intracellular shift causes serum depletion.
Without prompt recognition, cardiac electrical instability can occur.
Fluid and Sodium Retention
Insulin also promotes:
- Renal sodium retention
- Water retention
This can lead to:
- Peripheral edema
- Pulmonary edema
- Heart failure in vulnerable patients
The registered nurse must monitor daily weights and intake/output carefully.
Thiamine Deficiency in Refeeding Syndrome
Thiamine (vitamin B1) is required for carbohydrate metabolism.
When carbohydrates are reintroduced:
- Thiamine demand increases
- Deficiency can worsen
This may lead to:
- Wernicke’s encephalopathy
- Neurologic deterioration
Thiamine supplementation is a preventive nursing bundle intervention.
Laboratory Findings
Classic findings include:
- Low phosphate
- Low potassium
- Low magnesium
- Elevated glucose
- Possible low calcium
The RN nurse should anticipate electrolyte replacement orders when refeeding begins.
Prevention: Nursing Bundle for Safe Refeeding
A structured refeeding nursing bundle includes:
1️⃣ Identify high-risk patients
2️⃣ Start nutrition slowly
3️⃣ Monitor electrolytes daily (or more frequently)
4️⃣ Replace phosphate proactively
5️⃣ Supplement thiamine before feeding
6️⃣ Monitor cardiac rhythm
7️⃣ Strict intake/output monitoring
Prevention is far safer than correction.
Treatment of Refeeding Syndrome
If electrolyte collapse occurs:
- Slow or pause nutritional support
- Replace phosphate IV or PO
- Replace potassium and magnesium
- Administer thiamine
- Continuous cardiac monitoring
The RN nurse plays a critical role in early detection and intervention.
Cardiac Complications
Electrolyte depletion increases risk for:
- Ventricular arrhythmias
- Prolonged QT
- Cardiac arrest
Hypophosphatemia weakens myocardial contraction, reducing cardiac output.
For the nurse, this is a life-threatening emergency requiring rapid escalation.
Respiratory Complications
Low phosphate weakens:
- Diaphragm function
- Intercostal muscles
This may result in:
- Hypoventilation
- Respiratory failure
- Need for mechanical ventilation
This complication is frequently emphasized in critical care nursing education.
NCLEX High-Yield Review
- Refeeding syndrome occurs after restarting nutrition
- Insulin causes intracellular electrolyte shift
- Phosphate is the most critical electrolyte
- High-risk patients must be monitored closely
- Start feeds slowly
- Always give thiamine before glucose in malnourished patients
If a severely malnourished patient develops weakness and arrhythmia after starting tube feeds, suspect refeeding syndrome.
Integrating Refeeding Knowledge into Nursing Practice
For the experienced registered nurse, refeeding syndrome is a preventable complication when recognized early.
Strong assessment skills, electrolyte interpretation, and use of a structured nursing bundle improve patient safety and reduce mortality.
Because endocrine and metabolic emergencies are heavily tested on the NCLEX, understanding refeeding syndrome strengthens both exam readiness and bedside confidence.
Final Thoughts
Refeeding syndrome represents a rapid electrolyte collapse triggered by insulin-driven cellular shifts. What appears to be simple nutritional support can quickly become a life-threatening emergency.
For every nurse and RN nurse, recognizing at-risk patients, monitoring electrolytes, and implementing preventive strategies are critical responsibilities in safe, evidence-based nursing care.
Early recognition saves lives.