A Practical NCLEX Guide for the Nurse, Registered Nurse, and RN Nurse
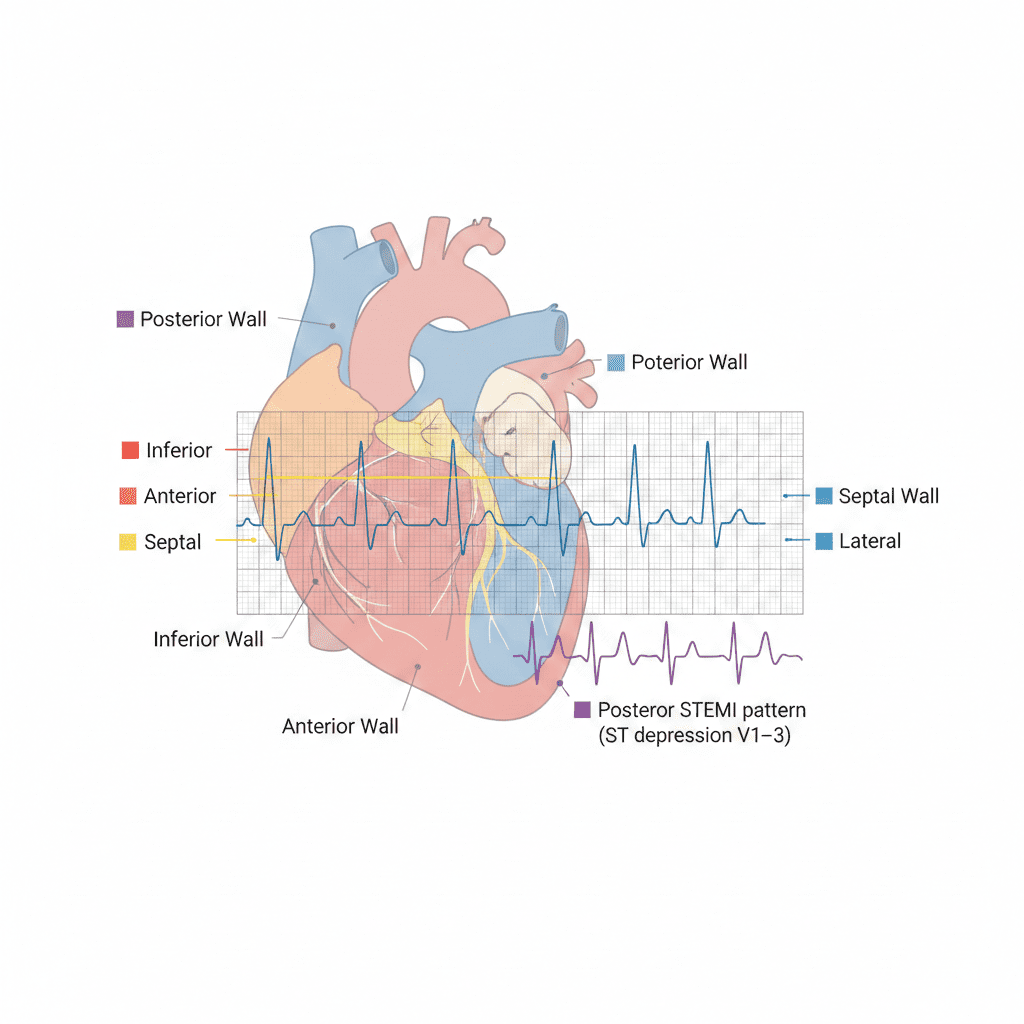
STEMI location is determined by identifying ST elevation in specific contiguous ECG leads—each lead group corresponds to a different wall of the heart.
For every nurse, registered nurse, and RN nurse, recognizing ST-elevation myocardial infarction (STEMI) patterns on a 12-lead ECG is a life-saving skill. Whether preparing for the NCLEX or working in emergency, telemetry, or ICU settings, understanding how to localize a STEMI strengthens rapid response and supports a structured cardiac nursing bundle.
Time is myocardium. Early recognition saves heart muscle.
What Defines a STEMI?
A STEMI occurs when there is complete coronary artery occlusion causing transmural (full-thickness) myocardial injury.
ECG Criteria for STEMI
STElevation≥1mmin2contiguousleadsST Elevation ≥1 mm in 2 contiguous leadsSTElevation≥1mmin2contiguousleads
(Thresholds vary slightly by lead and patient characteristics, but this is the core NCLEX standard.)
For the bedside nurse, this means:
- Look for ST elevation
- Confirm it appears in at least two neighboring leads
- Identify which region those leads represent
Step 1: Group the 12 Leads by Heart Wall
The 12-lead ECG is divided into anatomical regions:
1️⃣ Inferior Wall STEMI
Leads:
II, III, aVF
These leads look at the inferior surface of the heart.
Common Culprit:
Right coronary artery (RCA)
Nursing Clues:
- Bradycardia (RCA supplies SA/AV node)
- Hypotension
- Possible right ventricular involvement
For the RN nurse, inferior STEMIs require close blood pressure monitoring and cautious nitrate use.
2️⃣ Anterior Wall STEMI
Leads:
V1, V2, V3, V4
These precordial leads examine the anterior wall.
Common Culprit:
Left anterior descending artery (LAD)
Often called the “widow-maker.”
Clinical Impact:
- Large infarct size
- High risk for cardiogenic shock
- Ventricular dysrhythmias
For the registered nurse, anterior STEMIs demand aggressive monitoring and rapid cath lab activation.
3️⃣ Septal STEMI
Leads:
V1, V2
These reflect the interventricular septum.
Common Culprit:
Proximal LAD
Septal involvement often accompanies anterior STEMI.
4️⃣ Lateral Wall STEMI
Leads:
I, aVL, V5, V6
These evaluate the lateral left ventricle.
Common Culprit:
Left circumflex artery (LCx)
For the cardiac nurse, lateral STEMIs may present with less dramatic symptoms but still require immediate intervention.
Step 2: Understand Contiguous Leads
Contiguous leads are anatomically next to each other.
Examples:
- II, III, aVF → Inferior group
- V1–V4 → Anterior/septal
- I, aVL → High lateral
- V5–V6 → Low lateral
This pattern recognition is frequently tested on the NCLEX.
Step 3: Recognize Reciprocal Changes
Reciprocal changes strengthen STEMI diagnosis.
Example:
Inferior STEMI (II, III, aVF ST elevation)
→ ST depression in I and aVL
For the experienced RN nurse, reciprocal changes confirm true injury rather than artifact.
Special Situation: Right Ventricular STEMI
If inferior STEMI is present:
Suspect right ventricular involvement.
Clues:
- ST elevation in V1
- Hypotension
- Clear lung sounds
- Elevated JVD
Right-sided ECG leads (V3R, V4R) may confirm diagnosis.
In the cardiac nursing bundle, avoid nitrates in RV infarction due to preload dependency.
Posterior STEMI: The Hidden MI
Posterior infarctions often show:
- ST depression in V1–V3
- Tall R waves
- Upright T waves
This is a mirror image of posterior ST elevation.
Posterior leads (V7–V9) confirm diagnosis.
For the registered nurse, recognizing posterior STEMI prevents dangerous delays.
Quick STEMI Localization Summary
| STEMI Location | Leads | Common Artery |
|---|---|---|
| Inferior | II, III, aVF | RCA |
| Anterior | V1–V4 | LAD |
| Septal | V1–V2 | LAD |
| Lateral | I, aVL, V5–V6 | LCx |
| Posterior | ST depression V1–V3 | RCA/LCx |
Nursing Bundle for Suspected STEMI
When a STEMI is identified:
- Activate STEMI protocol immediately
- Obtain IV access
- Administer oxygen if indicated
- Prepare for antiplatelet therapy per order
- Continuous cardiac monitoring
- Prepare for emergent PCI
Door-to-balloon time goal: ≤90 minutes.
This rapid-response cardiac nursing bundle is essential in emergency and ICU practice.
High-Yield NCLEX Pearls
✔️ ST elevation must appear in 2 contiguous leads
✔️ Inferior STEMI = II, III, aVF
✔️ Anterior STEMI = V1–V4
✔️ Reciprocal changes support diagnosis
✔️ LAD occlusion carries high mortality
The NCLEX frequently tests lead grouping and artery correlation.
Advanced Clinical Insight for the RN Nurse
Recognizing STEMI location helps anticipate complications:
- Inferior → Bradyarrhythmias
- Anterior → Cardiogenic shock
- Septal → Conduction blocks
- Lateral → Mitral regurgitation
- Posterior → Missed diagnosis risk
An expert nurse does not just identify ST elevation — they anticipate what happens next.
Final Thoughts for the Nurse and Registered Nurse
Recognizing STEMI location using the 12-lead ECG is a foundational cardiac skill.
It improves:
- Rapid intervention
- Communication with cardiology
- Clinical prioritization
- Patient survival
For NCLEX preparation and real-world cardiac nursing, mastering lead localization transforms ECG interpretation from memorization to meaningful clinical insight.
When you see ST elevation —
Don’t just call it a STEMI.
Call its location.
Because location predicts outcome.