Potassium imbalances are among the most dangerous electrolyte disturbances encountered in clinical practice. For every nurse, especially the ICU registered nurse (RN nurse), understanding why potassium shifts during acid-base disorders is critical for preventing cardiac complications. Because potassium and acid-base balance are heavily tested on the NCLEX, mastering these mechanisms strengthens both exam readiness and advanced nursing practice.
Potassium is not just an electrolyte — it is a determinant of cardiac electrical stability.
Why Potassium Matters at the Cellular Level
Normal serum potassium range:
3.5–5.0 mEq/L
About 98% of potassium is located inside cells. Only 2% circulates in the bloodstream.
This delicate gradient is maintained by:
- The Na⁺/K⁺ ATPase pump
- Cell membrane permeability
- Acid-base balance
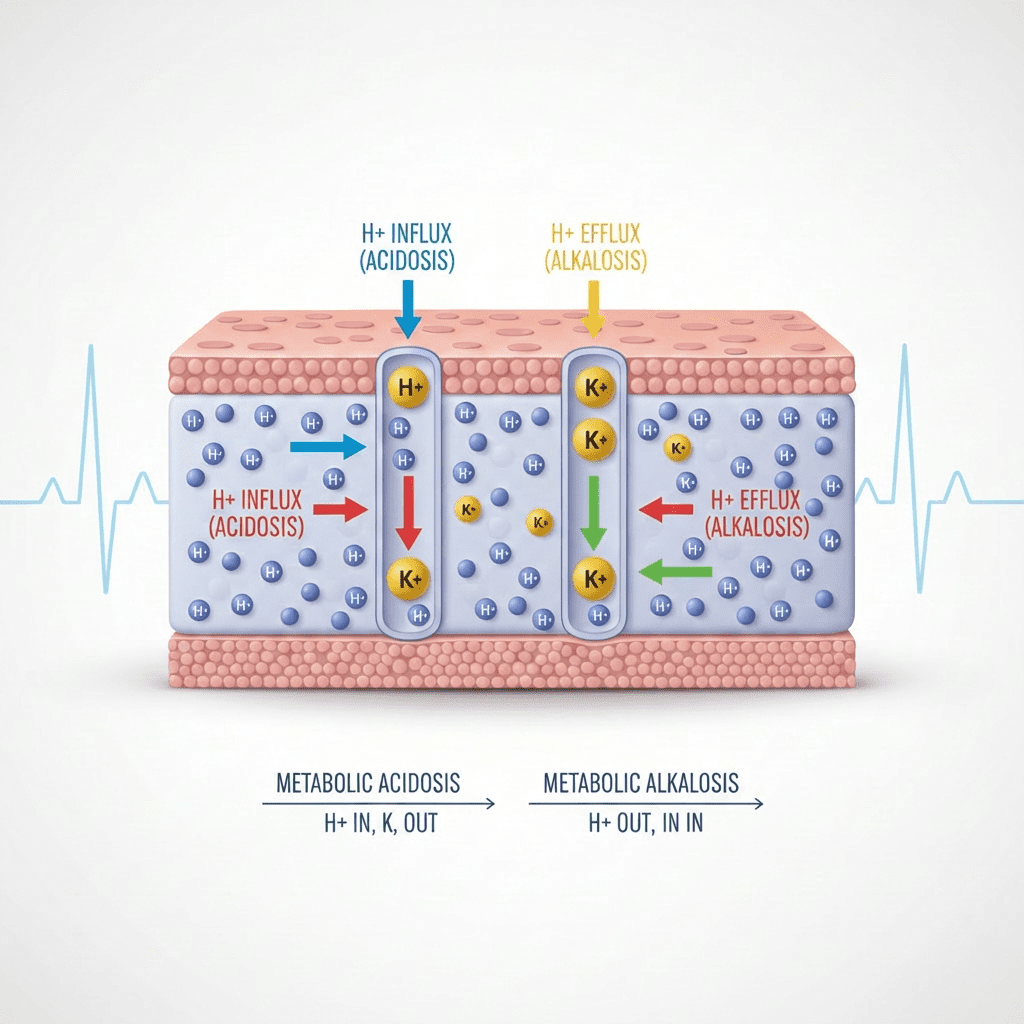
Acid-base imbalances cause hydrogen ions and potassium ions to shift across cell membranes in opposite directions.
Understanding this ion exchange is key for every RN nurse managing critically ill patients.
The Core Mechanism: Hydrogen-Potassium Exchange
When the body experiences acid-base disturbances, hydrogen ions (H⁺) move in or out of cells to maintain pH balance.
To preserve electrical neutrality:
- When H⁺ enters a cell → K⁺ exits
- When H⁺ exits a cell → K⁺ enters
This ion shift explains most potassium changes during acid-base disorders.
Potassium in Metabolic Acidosis
What Happens?
In metabolic acidosis:
- Excess hydrogen ions accumulate in the blood
- H⁺ moves into cells
- Potassium moves out of cells
- Serum potassium rises
Result: Hyperkalemia
Cellular Explanation
The body attempts to buffer excess acid by shifting H⁺ into cells. To maintain electrochemical balance, potassium exits the cell into the bloodstream.
This does not necessarily mean total body potassium is elevated — it may simply be redistributed.
For the registered nurse, this distinction is critical.
Clinical Implications
Hyperkalemia can cause:
- Peaked T waves
- Widened QRS
- Cardiac arrhythmias
- Muscle weakness
On the NCLEX, metabolic acidosis is frequently associated with hyperkalemia.
The RN nurse must immediately assess cardiac rhythm.
Potassium in Metabolic Alkalosis
What Happens?
In metabolic alkalosis:
- Hydrogen ion levels decrease
- H⁺ exits cells
- Potassium moves into cells
- Serum potassium falls
Result: Hypokalemia
Cellular Explanation
To correct alkalosis, H⁺ leaves the cell. Potassium shifts into cells to maintain neutrality.
Serum potassium drops, even if total body potassium is normal.
Clinical Implications
Hypokalemia can cause:
- Flattened T waves
- U waves
- Muscle cramps
- Ileus
- Arrhythmias
The nurse must monitor ECG and assess neuromuscular status.
Respiratory Acid-Base Disorders and Potassium
Potassium shifts are more pronounced in metabolic disorders than respiratory disorders.
Why?
Respiratory changes affect CO₂ levels, which diffuse rapidly and are buffered differently. The potassium shift is less dramatic compared to metabolic acidosis or alkalosis.
On the NCLEX, metabolic disorders are more strongly linked to potassium abnormalities.
Diabetic Ketoacidosis (DKA): A Critical Example
DKA is a classic high-yield example for both ICU nursing and the NCLEX.
In DKA:
- Severe metabolic acidosis occurs
- Potassium shifts out of cells
- Serum potassium may appear normal or high
However, total body potassium is actually depleted due to osmotic diuresis.
When insulin is administered:
- Potassium moves back into cells
- Serum potassium can drop rapidly
The RN nurse must monitor potassium closely during insulin therapy.
The Role of Insulin in Potassium Shifts
Insulin stimulates the Na⁺/K⁺ ATPase pump, driving potassium into cells.
This is why insulin is used to treat hyperkalemia.
For the registered nurse, understanding this mechanism improves medication safety and patient monitoring.
Kidney Function and Potassium Regulation
The kidneys regulate potassium through:
- Aldosterone secretion
- Renal excretion
In acidosis:
- Kidneys may retain potassium
- Excretion decreases
In alkalosis:
- Potassium loss may increase
Renal dysfunction complicates acid-base related potassium shifts.
ECG Changes: High-Yield Nursing Assessment
Potassium imbalance can rapidly become life-threatening.
The RN nurse should monitor for:
Hyperkalemia
- Peaked T waves
- Wide QRS
- Bradycardia
Hypokalemia
- U waves
- ST depression
- Ventricular arrhythmias
Cardiac monitoring is part of a critical nursing bundle for electrolyte management.
Potassium Correction: Nursing Considerations
Treating Hyperkalemia
- Calcium gluconate (cardiac stabilization)
- Insulin + glucose
- Sodium bicarbonate (if acidosis present)
- Diuretics
- Dialysis
Treating Hypokalemia
- Oral or IV potassium replacement
- Correct underlying alkalosis
- Monitor magnesium levels
The RN nurse must never administer IV potassium as a rapid IV push.
This is a common NCLEX safety question.
Nursing Bundle for Potassium Imbalance
A structured nursing bundle approach includes:
- Continuous cardiac monitoring
- Frequent electrolyte labs
- Acid-base assessment (ABGs)
- Strict intake and output
- Medication review (diuretics, insulin)
- Renal function monitoring
Consistency prevents adverse events.
Acid-Base and Potassium: NCLEX Summary Table
| Disorder | Hydrogen Movement | Potassium Movement | Serum K⁺ |
|---|---|---|---|
| Metabolic Acidosis | Into cell | Out of cell | High |
| Metabolic Alkalosis | Out of cell | Into cell | Low |
Remember:
Acidosis → Hyperkalemia
Alkalosis → Hypokalemia
Why This Matters for Critical Care Nursing
Potassium shifts can occur rapidly and without warning. The experienced registered nurse anticipates electrolyte changes whenever an acid-base imbalance is present.
Understanding the deep cellular mechanisms allows the RN nurse to:
- Anticipate lab trends
- Recognize ECG changes early
- Prevent cardiac arrest
- Improve patient outcomes
This knowledge strengthens both ICU performance and NCLEX preparation.
Final Thoughts
Potassium shifts in acid-base disorders are driven by hydrogen ion exchange at the cellular level. While lab values provide clues, understanding the underlying physiology gives nurses true clinical insight.
For every nurse and registered nurse, mastering potassium movement during acidosis and alkalosis is essential for safe and effective nursing care.
Because electrolyte and acid-base management are heavily emphasized on the NCLEX, deep comprehension of potassium dynamics enhances both exam confidence and bedside expertise.
In critical care nursing, recognizing a potassium shift early can save a life.