When a patient experiences cardiac arrest, survival doesn’t end with return of spontaneous circulation (ROSC). The post–cardiac arrest phase is critical and requires skilled nursing interventions to optimize neurological recovery and prevent complications. For every registered nurse (RN) and nursing student preparing for the NCLEX, understanding Post–Cardiac Arrest Care and Targeted Temperature Management (TTM) is vital for both clinical excellence and exam success.
💓 What Is Post–Cardiac Arrest Care?
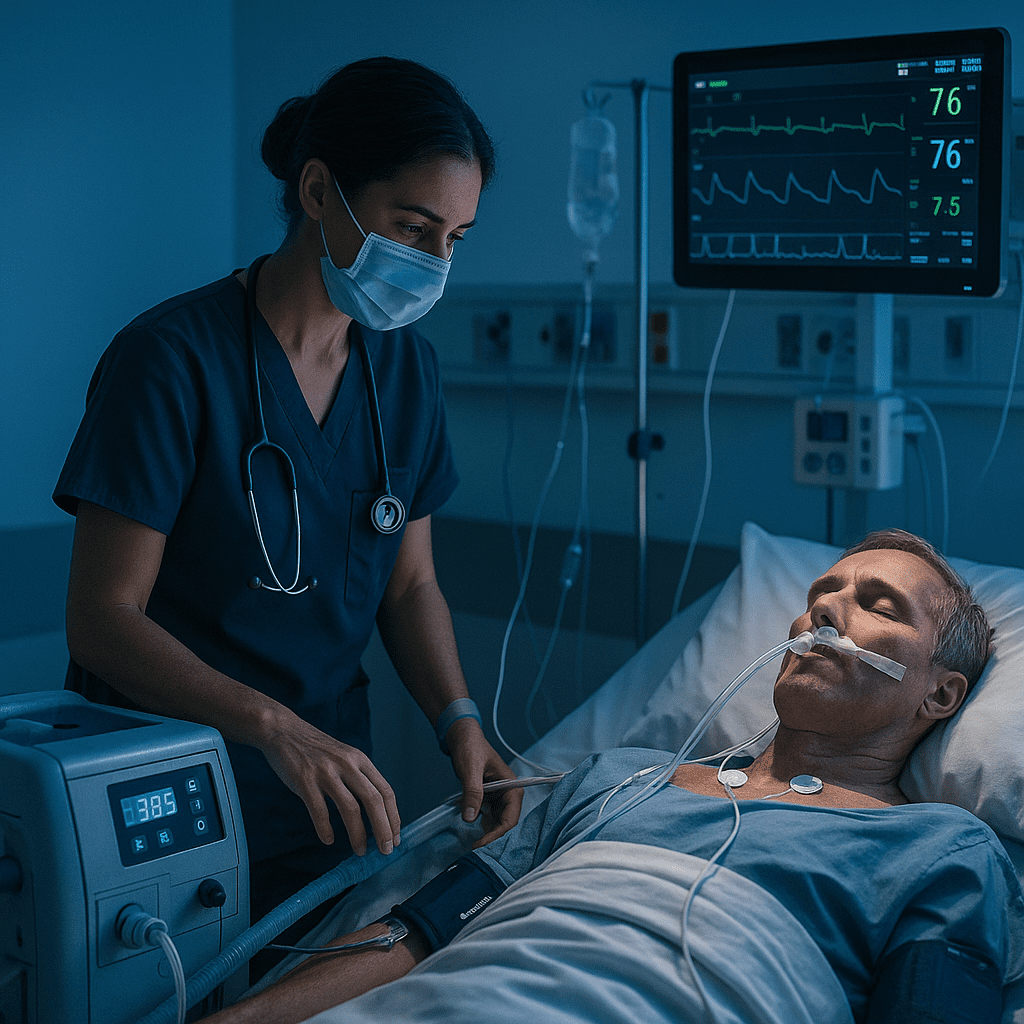
Post–cardiac arrest care is a structured, multidisciplinary process focused on stabilizing patients after ROSC. It aims to restore hemodynamic stability, prevent recurrent arrest, and protect vital organs — especially the brain.
For nurses, this stage is where rapid assessment, accurate documentation, and evidence-based interventions truly matter. RNs are central to the monitoring, coordination, and implementation of care bundles in this delicate recovery phase.
🧊 Understanding Targeted Temperature Management (TTM)
Targeted Temperature Management (TTM), formerly known as therapeutic hypothermia, is the controlled cooling of a patient’s body temperature (typically to 32–36°C) for 24–48 hours after cardiac arrest.
The goal: minimize neurological injury and reduce metabolic demand in the brain.
Key Phases of TTM for Nurses to Know:
- Induction: Cooling the patient to target temperature.
- Maintenance: Sustaining target temperature (32–36°C).
- Rewarming: Slow and controlled rewarming (0.25–0.5°C per hour).
🩺 Nursing Priorities in Post–Cardiac Arrest Care
Registered nurses play a vital role in every stage of care. Here’s what every RN nurse should prioritize:
1. Airway, Breathing, and Circulation (ABCs)
- Ensure adequate oxygenation (SpO₂ > 94%).
- Maintain appropriate blood pressure (MAP ≥ 65 mmHg).
- Use vasopressors or fluids as ordered to stabilize hemodynamics.
2. Neurological Monitoring
- Assess level of consciousness using the Glasgow Coma Scale (GCS).
- Monitor for seizure activity.
- Support sedation and analgesia during TTM to prevent shivering.
3. Temperature Management
- Set up cooling devices (surface or intravascular).
- Monitor temperature continuously.
- Avoid rapid rewarming to prevent rebound hyperthermia.
4. Hemodynamic Stability
- Continuous ECG and invasive BP monitoring.
- Administer IV fluids and vasoactive agents per protocol.
- Monitor for arrhythmias (especially bradycardia during cooling).
5. Glycemic and Electrolyte Control
- Regular blood glucose checks (target 140–180 mg/dL).
- Watch for hypokalemia, hypomagnesemia, or hypophosphatemia — common during cooling.
6. Prevent Infection
- Maintain strict aseptic technique for lines, tubes, and catheters.
- Monitor white blood cell count and temperature closely.
💊 Medications Commonly Used
- Sedatives: Propofol, midazolam
- Analgesics: Fentanyl, morphine
- Paralytics: Vecuronium (to prevent shivering)
- Vasoactive Drugs: Norepinephrine, dopamine for blood pressure support
- Anticonvulsants: Levetiracetam if seizures occur
Nurses must understand medication timing, compatibility, and titration — all of which are NCLEX-relevant nursing responsibilities.
🧠 NCLEX Nursing Tips
For NCLEX-style questions, focus on priority actions and patient safety:
- Always maintain airway and circulation first.
- Prevent shivering during TTM (as it increases oxygen demand).
- Rewarm slowly — rapid rewarming can cause hypotension or arrhythmias.
- Monitor for electrolyte shifts during temperature transitions.
- Document every phase meticulously — an essential part of the nursing bundle.
📋 Nursing Bundle for Post–Cardiac Arrest Care
Many hospitals use standardized nursing bundles for cardiac arrest recovery, which typically include:
- Continuous temperature monitoring
- Sedation and pain control
- Hemodynamic optimization
- Seizure prevention
- Glucose and electrolyte control
- Family communication and emotional support
These evidence-based steps are part of what every registered nurse and RN nurse should know when delivering critical care or preparing for the NCLEX exam.
💬 Final Thoughts
Post–Cardiac Arrest Care and Targeted Temperature Management require precise coordination, critical thinking, and compassionate nursing practice. Every registered nurse must be skilled in balancing advanced technology with holistic patient care — ensuring the best possible neurological outcomes.
❓ FAQ: Post–Cardiac Arrest Care and Targeted Temperature Management (TTM)
The primary goal of post–cardiac arrest care is to stabilize the patient after return of spontaneous circulation (ROSC), protect brain function, prevent complications, and improve survival outcomes. Nurses play a key role in continuous monitoring, documentation, and early intervention to optimize recovery.
The target temperature typically ranges from 32°C to 36°C (89.6°F–96.8°F). The exact target depends on hospital protocol, but maintaining a consistent temperature within this range helps minimize brain injury and metabolic demand.
TTM is usually maintained for 24 to 48 hours, followed by a slow rewarming phase (0.25–0.5°C per hour). RNs must ensure that the rewarming process is gradual to avoid complications such as hypotension and electrolyte imbalances.
Shivering increases oxygen consumption and counteracts cooling efforts. Nurses should use sedatives, analgesics, and sometimes paralytics to control shivering and maintain the target temperature effectively.