Phosphate is often overlooked compared to potassium or sodium, yet in the ICU it can become a silent threat. For every nurse, especially the critical care registered nurse (RN nurse), understanding phosphate imbalance is essential for preventing respiratory failure, cardiac instability, and neuromuscular collapse. Because electrolyte disorders are heavily tested on the NCLEX, phosphate disturbances are a high-yield topic in advanced nursing practice.
Severe hypophosphatemia in ICU patients can cause respiratory muscle failure, decreased cardiac output, and life-threatening complications.
Normal Phosphate Levels
Normal serum phosphate:
2.5–4.5 mg/dL
Phosphate is critical for:
- ATP production
- Cellular energy metabolism
- Oxygen delivery (2,3-DPG in red blood cells)
- Muscle contraction
- Neurologic function
- Acid-base buffering
In critically ill patients, phosphate levels can shift rapidly.
Why ICU Patients Are at High Risk
ICU patients frequently experience:
- Sepsis
- Trauma
- Major surgery
- Mechanical ventilation
- Malnutrition
- Refeeding
- Renal failure
These conditions disrupt normal phosphate regulation.
The RN nurse must anticipate instability rather than react to it.
Hypophosphatemia in ICU Patients
Causes
Common ICU causes include:
- Refeeding syndrome
- Sepsis
- Diabetic ketoacidosis treatment
- Alcohol withdrawal
- Continuous renal replacement therapy (CRRT)
- Respiratory alkalosis
Phosphate often shifts intracellularly during recovery phases.
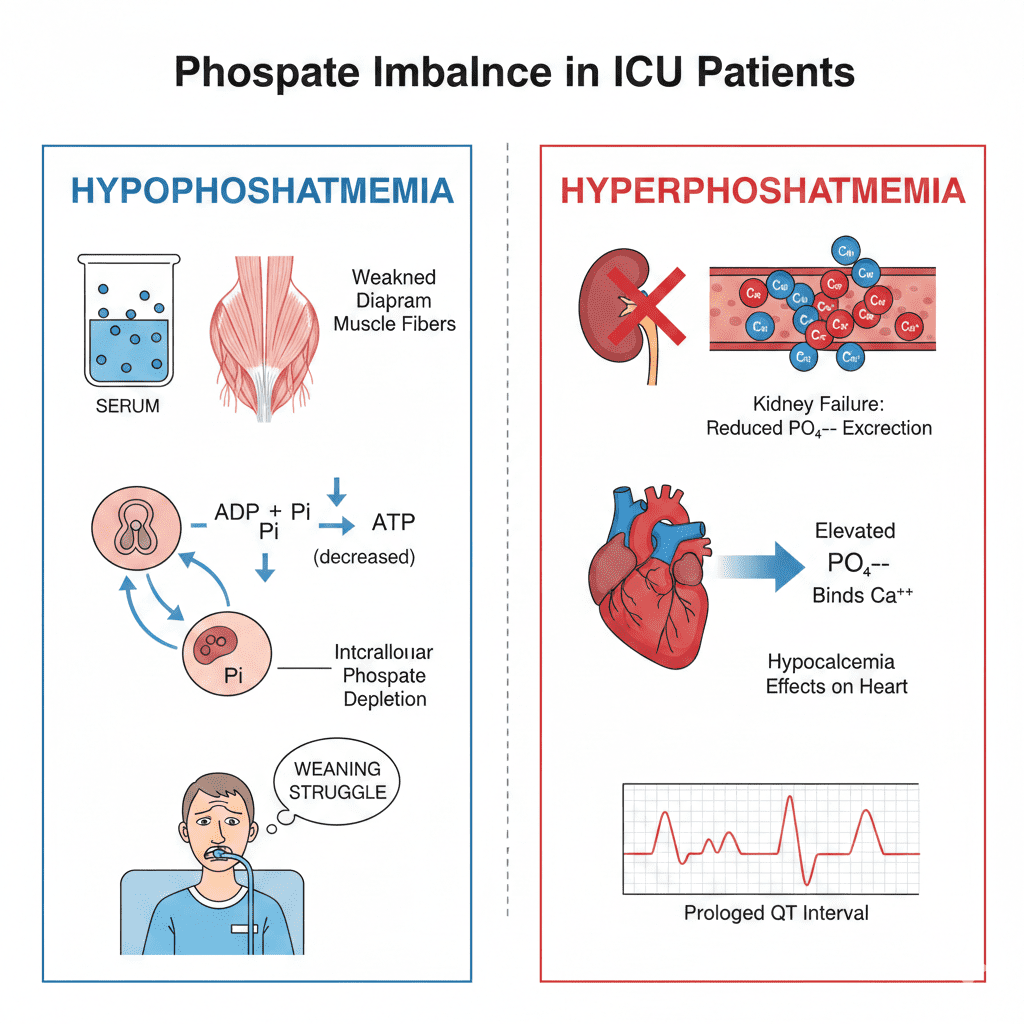
Why Low Phosphate Is Dangerous
Phosphate is required to produce ATP.
When phosphate drops:
- Energy production decreases
- Muscle contraction weakens
- Diaphragm function declines
- Cardiac contractility decreases
In the ICU, this can result in:
- Failure to wean from ventilator
- Hypotension
- Arrhythmias
- Altered mental status
The registered nurse must connect unexplained weakness with possible hypophosphatemia.
Respiratory Failure and Phosphate
One of the most critical complications:
Low phosphate → weak diaphragm → hypoventilation.
If a ventilated patient repeatedly fails spontaneous breathing trials, check phosphate.
This concept is frequently emphasized in NCLEX critical care questions.
Cardiac Effects of Hypophosphatemia
Low phosphate can cause:
- Decreased myocardial contractility
- Reduced cardiac output
- Ventricular arrhythmias
Although ECG changes are less specific than potassium disorders, cardiac monitoring is still essential.
Hyperphosphatemia in ICU Patients
Causes
- Acute kidney injury
- End-stage renal disease
- Tumor lysis syndrome
- Rhabdomyolysis
- Massive tissue breakdown
When kidneys fail, phosphate accumulates.
Consequences of High Phosphate
Elevated phosphate binds calcium.
This leads to:
- Hypocalcemia
- Tetany
- Prolonged QT interval
- Secondary hyperparathyroidism
Chronic elevation causes:
- Vascular calcification
- Organ dysfunction
The nurse must monitor calcium and phosphate together.
Phosphate and Acid-Base Balance
Phosphate acts as an intracellular buffer.
In metabolic acidosis:
- Phosphate shifts may worsen
- Renal clearance decreases
Understanding this relationship strengthens ICU nursing assessment skills.
Refeeding Syndrome and ICU Monitoring
Critically ill malnourished patients are at high risk.
When feeding begins:
- Insulin increases
- Phosphate shifts into cells
- Serum phosphate drops rapidly
This is why ICU protocols often include daily electrolyte monitoring during refeeding.
A structured electrolyte nursing bundle improves patient safety.
Laboratory Trends to Monitor
The RN nurse should monitor:
- Serum phosphate
- Calcium
- Magnesium
- Potassium
- Renal function (BUN, creatinine)
- Arterial blood gases
Electrolytes interact — they rarely shift alone.
Treatment of Hypophosphatemia
Mild Cases
- Oral phosphate replacement
Severe Cases (<1.0 mg/dL)
- IV phosphate replacement
- Continuous cardiac monitoring
IV phosphate must be administered cautiously.
The registered nurse must monitor:
- Infusion rate
- Serum calcium
- Renal function
- Telemetry
Rapid infusion may cause hypocalcemia.
Treatment of Hyperphosphatemia
Management includes:
- Phosphate binders
- Dialysis (if renal failure)
- Treating underlying cause
Phosphate binders must be given with meals.
This is a classic NCLEX teaching point.
Nursing Bundle for ICU Phosphate Management
A structured ICU nursing bundle includes:
1️⃣ Daily phosphate monitoring
2️⃣ Ventilator weaning assessment
3️⃣ Cardiac rhythm monitoring
4️⃣ Renal function evaluation
5️⃣ Nutrition monitoring
6️⃣ Safe IV replacement protocol
7️⃣ Patient and family education when appropriate
Standardized monitoring prevents complications.
Clinical Scenario (NCLEX Thinking)
A malnourished ICU patient begins tube feeding and develops weakness and difficulty weaning from the ventilator.
Most likely cause?
→ Hypophosphatemia.
This scenario frequently appears in NCLEX questions.
Why Phosphate Is Often Missed
Unlike potassium:
- Symptoms are subtle
- ECG changes are less dramatic
- Lab monitoring may be less frequent
But in critical illness, phosphate can determine ventilator success or failure.
The RN nurse must advocate for comprehensive electrolyte review.
NCLEX High-Yield Review
- Normal phosphate: 2.5–4.5 mg/dL
- Low phosphate → respiratory failure
- High phosphate → low calcium
- Refeeding causes phosphate shift
- Monitor ICU patients closely
- Give phosphate binders with meals
If a ventilated patient has unexplained weakness, check phosphate.
Integrating Phosphate Knowledge into Nursing Practice
For every nurse and experienced RN nurse, phosphate monitoring is essential in ICU care.
Understanding its role improves:
- Ventilator management
- Cardiac monitoring
- Nutritional therapy
- Renal care
- NCLEX exam readiness
A proactive electrolyte nursing bundle approach ensures early detection and safer outcomes.
Final Thoughts
Phosphate imbalance in ICU patients can quietly progress to life-threatening complications. From respiratory failure to cardiac instability, phosphate disturbances demand careful monitoring and rapid intervention.
For every registered nurse, mastering this electrolyte strengthens critical care expertise and improves nursing practice at the bedside.
In the ICU, energy is life — and phosphate powers that energy.