When a patient goes into cardiac arrest, nurses must know exactly what they’re seeing on the monitor — and more importantly, what it really means.
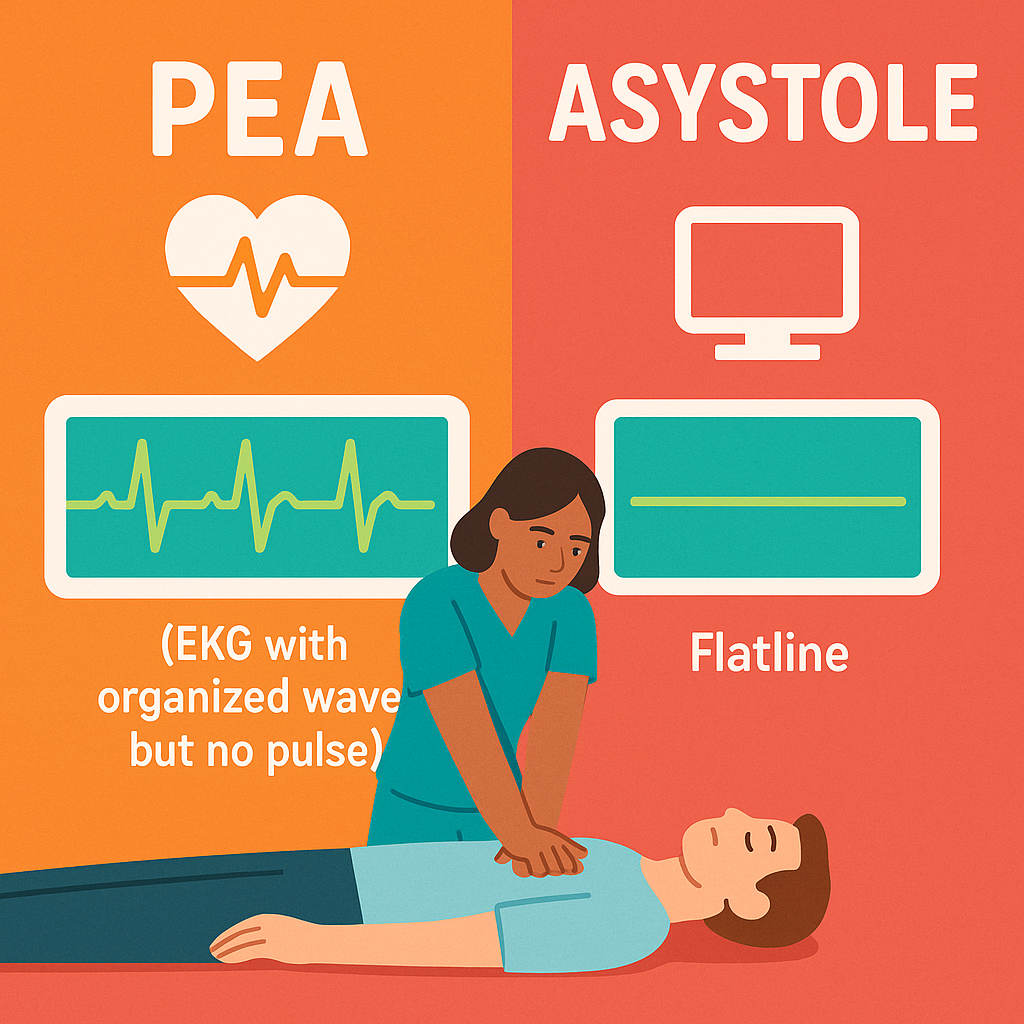
Two of the most confusing heart rhythms during a code are PEA (Pulseless Electrical Activity) and Asystole.
At first glance, they might seem similar because both mean no pulse. However, only one shows electrical activity on the monitor.
In this guide, we’ll explore how to tell them apart, why that difference matters, and what immediate steps nurses must take for each.
❤️ What Is PEA?
To begin with, PEA means the heart’s electrical system is still firing, yet the heart muscle isn’t contracting effectively enough to create a pulse. In other words, you’ll see an EKG tracing — but no actual circulation.
👉 Key point: PEA is not a single rhythm; it’s a clinical condition.
You might see normal sinus rhythm, severe bradycardia, or even tachycardia, but the patient will have no pulse strong enough to sustain blood flow.
🔍 How PEA Looks on an EKG
- Any organized rhythm (normal, brady, or tachy)
- P waves and QRS complexes may appear normal
- However, when you check the patient, there’s no pulse!
🔬 What Causes PEA?
PEA occurs when there’s a disconnect between electrical activity and mechanical pumping. Basically, the electrical signals are present, but something prevents the heart muscle from responding.
Common causes include:
- Severe hypovolemia (low blood volume)
- Massive pulmonary embolism (PE)
- Cardiac tamponade (fluid around the heart)
- Tension pneumothorax
- Severe hypoxia
- Electrolyte imbalances (especially hyperkalemia)
- Acidosis
- Drug overdose
To make it easier, nurses remember these using the 5 H’s and 5 T’s:
- H’s: Hypovolemia, Hypoxia, Hydrogen ions (acidosis), Hypo/hyperkalemia, Hypothermia
- T’s: Tension pneumothorax, Tamponade, Toxins, Thrombosis (MI or PE), Trauma
Therefore, identifying and correcting these causes is the real treatment for PEA.
❤️ What Is Asystole?
In contrast, Asystole means there is no electrical activity at all — the heart is completely silent, both electrically and mechanically.
It is quite literally a flatline.
👉 Key point: Asystole occurs when the heart’s pacemaker cells have stopped firing.
Consequently, there’s no impulse and no contraction.
🔍 How Asystole Looks on an EKG
- A flat, straight line
- No P waves, no QRS complexes, no spikes
- Always double-check, since a loose lead can mimic asystole!
🔬 What Causes Asystole?
Usually, Asystole means the heart’s electrical and muscular systems have completely failed.
Often, it follows prolonged cardiac arrest or severe myocardial damage.
Common causes include:
- Prolonged cardiac arrest
- Untreated ventricular fibrillation or PEA
- Massive myocardial infarction (MI)
- End-stage heart failure
- Severe trauma
- Terminal illness
As a result, the prognosis is typically poor — but immediate, high-quality CPR can still make a difference.
💡 How to Tell the Difference: PEA vs. Asystole
| Feature | PEA | Asystole |
|---|---|---|
| EKG | Organized rhythm | Flat line |
| Pulse | None | None |
| Electrical Activity | Yes | No |
| Treatable Causes | Usually yes | Rare (end-stage) |
| Defibrillation? | No | No |
In short, PEA has electrical activity without a pulse, while Asystole has neither.
🩺 What Should Nurses Do for PEA?
When you identify PEA, follow these critical steps:
1️⃣ Check responsiveness and pulse – Confirm true pulselessness.
2️⃣ Call a Code Blue immediately.
3️⃣ Start high-quality CPR without delay.
4️⃣ Do NOT defibrillate – PEA is not a shockable rhythm.
5️⃣ Administer epinephrine every 3–5 minutes as per ACLS.
6️⃣ Search for reversible causes – The 5 H’s and 5 T’s are your roadmap.
Meanwhile, the nurse should:
- Run the code alongside the team
- Draw labs quickly
- Give IV fluids if hypovolemia is suspected
- Prepare for needle decompression if tension pneumothorax is possible
- Support with medications and airway management
Therefore, teamwork and fast identification of the cause can truly save a life.
🩺 What Should Nurses Do for Asystole?
Similarly, when you detect Asystole, proceed carefully but efficiently:
1️⃣ Check all leads and connections – Ensure it’s real Asystole, not artifact.
2️⃣ If confirmed and pulseless, call a Code Blue right away.
3️⃣ Begin high-quality CPR immediately.
4️⃣ Give epinephrine every 3–5 minutes.
5️⃣ Do NOT defibrillate – shocking a flatline is ineffective.
During the code, nurses should:
- Provide compressions or manage the airway
- Prepare medications on schedule
- Document every action
- Communicate clearly with the code team
Although Asystole carries a poor prognosis, prompt CPR and correction of reversible causes offer the best chance of survival.
🔑 Key Differences in Treatment
| Action | PEA | Asystole |
|---|---|---|
| Defibrillate? | ❌ No | ❌ No |
| CPR? | ✅ Yes | ✅ Yes |
| Epinephrine? | ✅ Yes | ✅ Yes |
| Find Cause? | ✅ Yes | ✅ Yes |
| Best Chance? | Fix underlying cause | Fix underlying cause |
Thus, both rhythms require CPR and epinephrine — but recovery depends entirely on treating the reversible cause.
💬 Why Understanding PEA vs. Asystole Matters
For nurses, recognizing these two rhythms quickly is critical. Otherwise, mistaking PEA for a shockable rhythm can waste valuable time, and missing the underlying cause can cost a life.
👉 Remember:
- PEA = treat the cause
- Asystole = keep CPR going, give epi, and confirm flatline
In other words, your ability to identify and act decisively during a code can truly change the outcome.
✅ Nursing Cheat Sheet
| Rhythm | EKG | Pulse | Shock? | Main Action |
|---|---|---|---|---|
| PEA | Organized rhythm | None | ❌ | CPR, epi, fix cause |
| Asystole | Flatline | None | ❌ | CPR, epi, confirm flatline |
🗝️ Conclusion
Ultimately, both PEA and Asystole indicate cardiac arrest, but only PEA shows an organized rhythm on the monitor.
Neither should be shocked, yet both demand immediate CPR, epinephrine, and a focused search for what went wrong.
For every nurse, understanding these two rhythms isn’t just an NCLEX topic — it’s a lifesaving skill.
By staying calm, thinking critically, and working as a team, you give your patient the best possible chance at survival.