For nursing students preparing for the NCLEX and for every registered nurse (RN nurse) at the bedside, understanding pacemaker strips is a critical skill. Nurses often encounter patients with pacemakers in telemetry units, critical care, and even medical-surgical floors. Recognizing pacemaker spikes and providing the right nursing care ensures both patient safety and accurate documentation.
🔹 What Is a Pacemaker?
A pacemaker is a medical device that sends small electrical impulses to the heart to maintain an adequate heart rate and rhythm. Patients with bradycardia, heart block, or certain dysrhythmias may require a permanent or temporary pacemaker.
For nurses studying with a nursing bundle or reviewing for the NCLEX, understanding pacemaker rhythms is a common exam topic.
🔹 Recognizing Pacemaker Spikes on EKG Strips
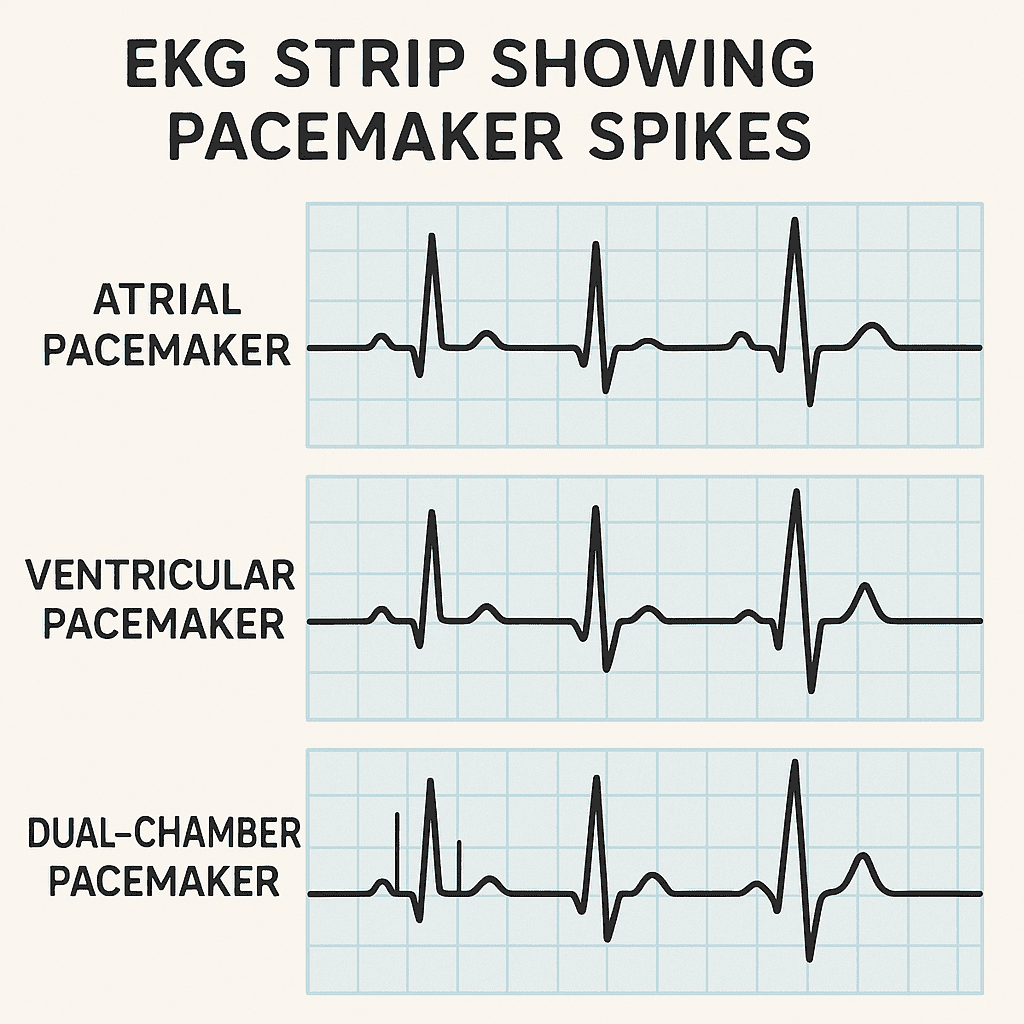
When reviewing an EKG, pacemaker spikes appear as thin vertical lines before specific waves, depending on the type of pacemaker.
- Atrial Pacemaker
- Spike appears before the P wave.
- Stimulates atrial contraction.
- Ventricular Pacemaker
- Spike appears before the QRS complex.
- Produces a wide QRS since the impulse is artificial.
- Dual-Chamber (AV) Pacemaker
- Two spikes: one before the P wave and another before the QRS complex.
💡 NCLEX tip for nurses: Always identify the location of the spike. It tells you whether the atria, ventricles, or both are being paced.
🔹 Normal vs. Abnormal Pacemaker Function
- ✅ Normal Function: Each pacemaker spike is followed by the appropriate wave (P or QRS).
- ⚠️ Failure to Capture: Spike occurs but no wave follows — the heart did not respond.
- ⚠️ Failure to Sense: Pacemaker fires inappropriately (e.g., spikes appear randomly without relation to cardiac cycle).
- ⚠️ Failure to Pace: No spikes appear even though the patient needs pacing.
These abnormal findings require immediate nurse intervention and communication with the provider.
🔹 Nursing Care for Patients with Pacemakers
1. Monitor the EKG Continuously
- Ensure pacing spikes are present and followed by appropriate complexes.
- Document any abnormal findings.
2. Assess the Patient, Not Just the Monitor
- Check pulse, blood pressure, oxygenation, and symptoms.
- Always correlate strip findings with patient condition.
3. Pacemaker Safety Teaching for Patients
- Avoid strong magnets (MRI, some phones, headphones).
- Report dizziness, chest pain, palpitations, or syncope.
- Keep scheduled device checks with cardiology.
4. Post-Implant Nursing Care
- Monitor insertion site for bleeding or infection.
- Restrict arm movement on the side of implant for a few weeks.
- Provide discharge teaching in simple language for families and patients.
💡 NCLEX nurse tip: Know the differences between failure to capture, failure to sense, and failure to pace. These terms frequently appear in NCLEX questions and clinical scenarios.
🔹 Final Thoughts
For the RN nurse, mastering pacemaker interpretation is vital. Recognizing pacemaker spikes and understanding nursing responsibilities ensures timely action and safe patient care. Whether studying in a nursing bundle for NCLEX or practicing at the bedside, always combine EKG knowledge with patient assessment.