Liver cirrhosis is a chronic, progressive condition that affects thousands of patients each year, and nurses play a critical role in managing its complications. For any RN nurse, registered nurse, or nursing student preparing for the NCLEX, understanding cirrhosis, its complications, and appropriate interventions is essential. This guide breaks down assessment cues, nursing priorities, and must-know interventions that appear frequently on NCLEX-style questions.
Whether you’re studying with a nursing bundle, preparing for exams, or caring for patients in clinical practice, this article provides everything you need.
⭐ Understanding Liver Cirrhosis
Cirrhosis occurs when healthy liver tissue becomes scarred, leading to impaired liver function. Over time, this scarring causes portal hypertension, decreased detoxification abilities, and metabolic imbalances. As a nurse, identifying complications early is crucial to prevent life-threatening consequences.
Major Complications of Cirrhosis & Nursing Responsibilities
Below are the most common complications seen in cirrhosis patients—high-yield NCLEX content—and the essential nursing interventions.
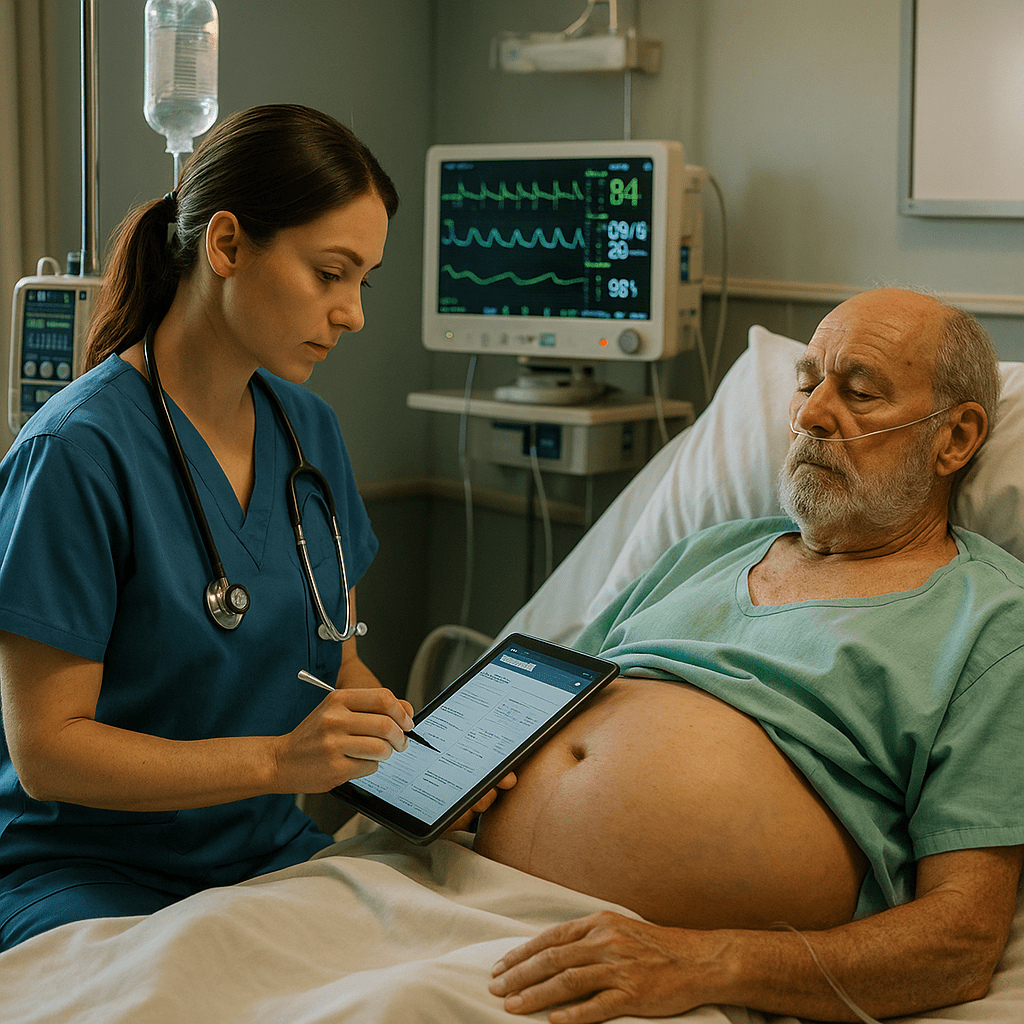
1. Ascites
Accumulation of fluid in the abdomen due to portal hypertension.
Assessment Findings
- Abdominal distention
- Shortness of breath
- Weight gain
- Fluid wave on exam
Nursing Interventions
- Monitor daily weights and abdominal girth
- Restrict sodium intake
- Educate about fluid restriction when ordered
- Administer diuretics (spironolactone, furosemide)
- Prepare for paracentesis if severe
- Assess for spontaneous bacterial peritonitis (SBP)—a major NCLEX question
2. Hepatic Encephalopathy
Buildup of ammonia due to impaired liver detoxification.
Assessment Findings
- Confusion, agitation, decreased LOC
- Asterixis (flapping tremor)
- Slurred speech
Nursing Interventions
- Administer lactulose to lower ammonia
- Monitor bowel movements (2–3/day needed)
- Avoid sedatives and narcotics
- Assess mental status frequently
- Teach the family to report confusion immediately
3. Esophageal Varices
Enlarged veins in the esophagus that can rupture due to portal hypertension.
Assessment Findings
- Hematemesis (vomiting blood)
- Melena
- Drop in blood pressure, tachycardia
Nursing Interventions
- Maintain airway during bleeding
- Prepare for endoscopic banding or sclerotherapy
- Administer vasopressin or octreotide
- Avoid NG tube insertion unless ordered—risk of bleeding
- Teach patients to avoid straining, alcohol, and NSAIDs
4. Jaundice
Yellowing of skin and sclera due to bilirubin buildup.
Nursing Interventions
- Monitor skin integrity and itching
- Provide antihistamines as ordered
- Use mild soap and moisturizers
- Assess liver labs (AST, ALT, bilirubin)
- Educate about avoiding alcohol completely
5. Coagulation Issues (Bleeding Risk)
Cirrhosis causes a reduced production of clotting factors.
Nursing Priorities
- Monitor PT, INR, platelets
- Avoid injections when possible
- Use soft toothbrush and avoid razors
- Prepare for vitamin K administration
6. Hepatorenal Syndrome
Life-threatening renal failure caused by severe liver damage.
Nursing Responsibilities
- Monitor I&O
- Track kidney labs (BUN, creatinine)
- Notify provider of decreased urine output
- Protect kidneys by avoiding nephrotoxic drugs
NCLEX Tips for Liver Cirrhosis
- Lactulose → lowers ammonia.
- No alcohol—ever.
- Low sodium diet reduces ascites.
- Varices = high risk → protect airway first.
- Monitor for sudden mental changes → ammonia levels rising.
These points appear repeatedly on NCLEX-style questions.
Patient Education for Long-Term Management
As an RN nurse, patient teaching is essential:
- Avoid alcohol permanently
- Follow a low-sodium diet
- Recognize symptoms of bleeding or confusion
- Take medications exactly as prescribed
- Attend follow-up appointments regularly
Patient teaching is a core NCLEX priority and a daily responsibility for every registered nurse.
Conclusion
Managing cirrhosis complications requires strong critical-thinking skills, rapid assessment, and effective intervention—skills that every nurse, whether a new graduate or an experienced RN nurse, must master. By understanding these core elements, you’re not only preparing effectively for the NCLEX, but also ensuring safer, more effective patient care.
FAQs: Nursing Role in Liver Cirrhosis Complications
Common complications include ascites, hepatic encephalopathy, esophageal varices, coagulopathy, portal hypertension, and hepatorenal syndrome. A registered nurse must assess these frequently because they often require rapid intervention and are heavily tested on the NCLEX.
Early signs include confusion, irritability, sleep-pattern changes, and asterixis (hand flapping). Nurses should monitor mental status closely and evaluate ammonia levels. Any sudden change should be reported immediately.
The priority is monitoring respiratory status, because fluid accumulation can impair breathing. Additionally, the nurse performs daily weights, tracks abdominal girth, monitors electrolytes, and evaluates response to diuretics.
A nurse must avoid inserting NG tubes unless ordered, educate patients to avoid straining, and monitor for black stools or vomiting blood. Beta-blockers are often prescribed; nurses reinforce medication adherence.