Maintaining a stable body temperature is one of the most critical needs of a newborn. Because infants have immature temperature control mechanisms, even small changes in the environment can lead to heat loss or overheating. The nurse plays a vital role in newborn thermoregulation through early assessment, preventive strategies, and ongoing monitoring. For nursing students, registered nurses, and RN nurses, this topic is frequently tested on the NCLEX.
This article reviews newborn thermoregulation, essential nursing interventions, and key NCLEX priorities.
Why Thermoregulation Is Critical in Newborn Nursing
Newborns lose heat quickly due to:
- Large body surface area
- Thin skin
- Limited subcutaneous fat
- Inability to shiver effectively
Cold stress increases oxygen consumption and glucose use, which can lead to hypoglycemia, metabolic acidosis, and respiratory distress. Therefore, thermoregulation is a core nursing responsibility.
Normal Newborn Temperature Range
The normal axillary temperature for a newborn is:
- 36.5°C–37.5°C (97.7°F–99.5°F)
The nurse should monitor temperature closely, especially during the first hours of life.
Mechanisms of Heat Loss
Understanding heat loss helps guide nursing interventions.
Four Ways Newborns Lose Heat:
- Evaporation – wet skin after birth
- Conduction – contact with cold surfaces
- Convection – exposure to cool air
- Radiation – heat loss to nearby cold objects
These mechanisms are high-yield NCLEX topics.
Immediate Nursing Interventions After Birth
Drying and Warming
The nurse should:
- Dry the newborn immediately
- Remove wet linens
- Use warm blankets
This prevents heat loss by evaporation.
Skin-to-Skin Contact
Placing the newborn skin-to-skin on the parent’s chest:
- Promotes thermoregulation
- Supports bonding
- Stabilizes heart rate and glucose levels
Skin-to-skin care is a best practice emphasized in nursing bundles.
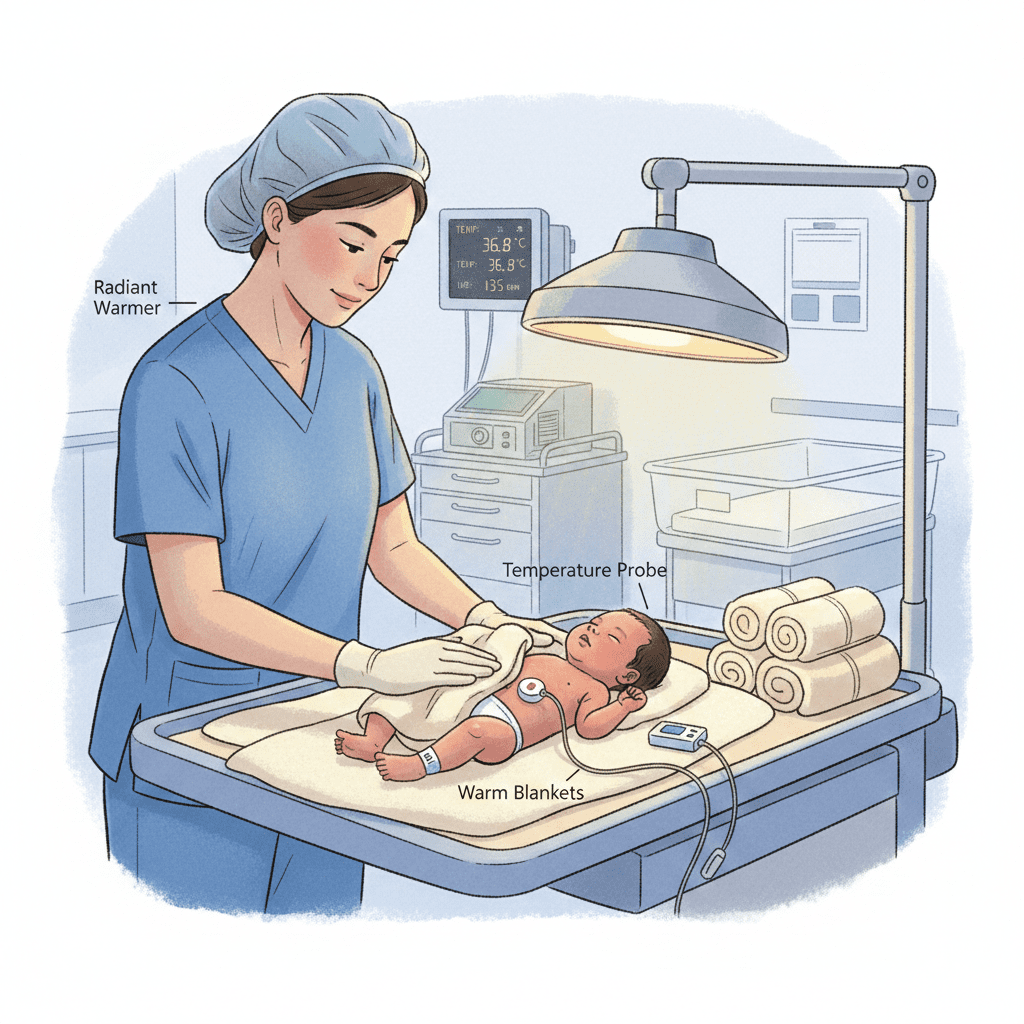
Use of Radiant Warmers and Incubators
When skin-to-skin is not possible, the RN nurse may use:
- Radiant warmers for immediate stabilization
- Incubators for ongoing temperature control
The nurse must monitor temperature frequently to avoid overheating.
Nursing Interventions During Routine Care
During assessments and procedures, the nurse should:
- Keep the newborn covered
- Warm hands and equipment
- Limit unnecessary exposure
These simple actions reduce heat loss and support thermal stability.
Recognizing Signs of Cold Stress
Early identification is essential.
Signs of Cold Stress Include:
- Cool extremities
- Poor feeding
- Lethargy
- Tachypnea
- Hypoglycemia
The registered nurse should respond promptly to prevent complications.
Preventing Overheating
While preventing cold stress is important, overheating is also harmful.
Nursing Strategies Include:
- Avoid excessive blankets
- Monitor temperature regularly
- Adjust environmental heat appropriately
Balanced thermoregulation is a key concept in neonatal nursing care.
Parent Education: A Nursing Priority
Nurses teach parents how to maintain newborn temperature at home.
Teaching Points:
- Appropriate clothing layers
- Safe sleep environment
- Avoid overheating
- Recognize signs of temperature instability
Education improves outcomes and supports safe newborn care.
NCLEX Tips: Newborn Thermoregulation
For NCLEX success, remember:
- Drying prevents evaporative heat loss
- Skin-to-skin is first-line intervention
- Cold stress increases oxygen and glucose use
- Hypothermia can cause hypoglycemia
- Nurses monitor temperature frequently
These concepts are commonly tested in pediatric and maternity nursing exams.
Final Thoughts
Newborn thermoregulation is a fundamental nursing responsibility that directly impacts infant survival and stability. Through timely interventions, vigilant monitoring, and parent education, the RN nurse plays a crucial role in maintaining thermal balance.