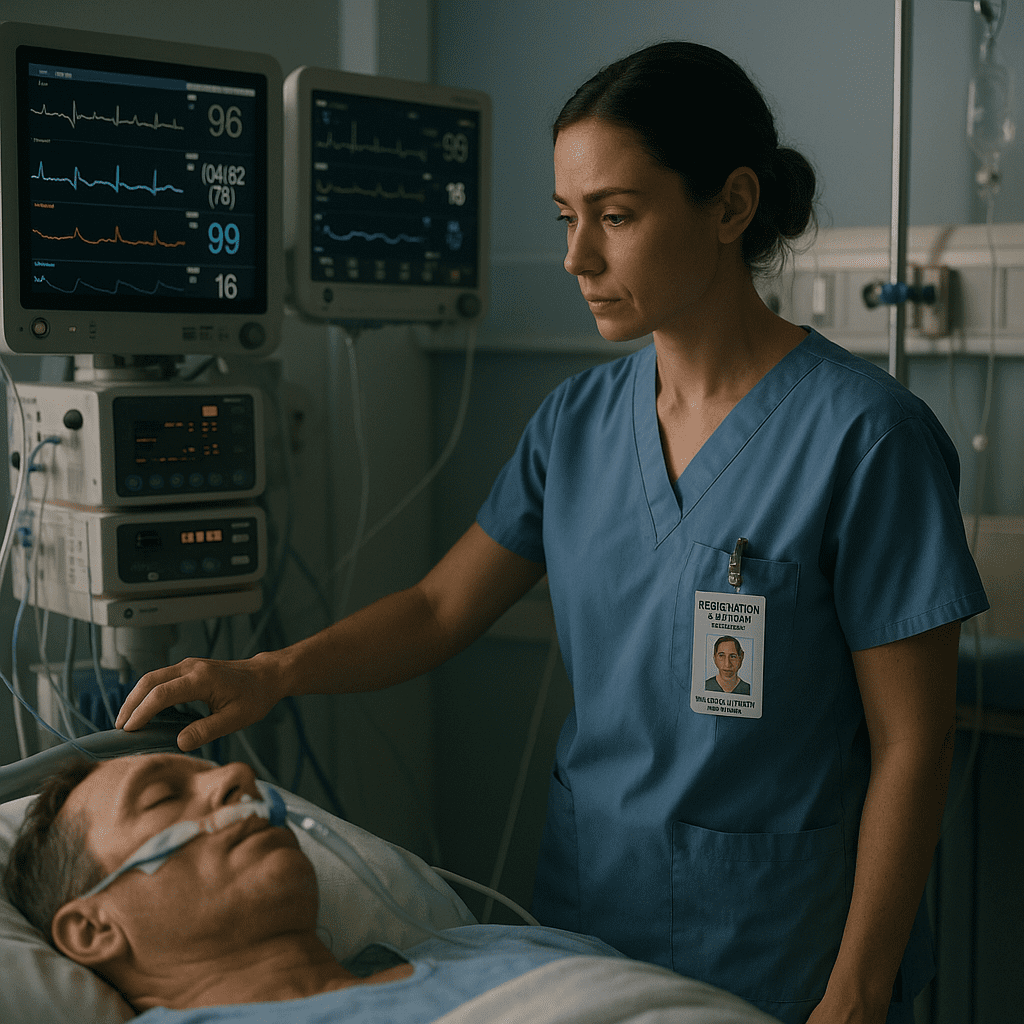
Multi-organ failure (MOF), also known as multiple organ dysfunction syndrome (MODS), is a life-threatening condition that occurs when two or more organ systems fail. For every registered nurse (RN nurse), early detection through careful monitoring is essential to improve patient outcomes. Understanding how to identify the warning signs and perform timely interventions is not only vital in critical care settings but also a key focus area for NCLEX preparation and clinical nursing practice.
🧠 Understanding Multi-Organ Failure
Multi-organ failure typically develops as a complication of sepsis, trauma, or shock. It can progress rapidly, making nursing assessment and continuous monitoring crucial. When one organ system begins to fail, others are at high risk of following due to impaired perfusion and oxygenation.
Common Causes:
- Severe infections (sepsis)
- Major trauma or burns
- Acute pancreatitis
- Prolonged hypotension or shock
- Cardiac arrest
For every nurse, recognizing these risk factors early can help prevent progression to full multi-organ failure.
❤️ Key Organs Affected and Their Warning Signs
1. Cardiovascular System
When the heart struggles to pump blood efficiently, perfusion to other organs decreases.
Signs to monitor:
- Hypotension or narrow pulse pressure
- Tachycardia or arrhythmias
- Decreased capillary refill
- Cool, clammy skin
Nursing Actions:
Monitor blood pressure continuously, assess for changes in skin temperature, and evaluate central venous pressure (CVP) if available.
2. Respiratory System
Respiratory failure often occurs early in MODS due to hypoxia or acute respiratory distress syndrome (ARDS).
Signs to monitor:
- Low oxygen saturation (SpO₂ < 90%)
- Increased work of breathing or use of accessory muscles
- Crackles or diminished lung sounds
- Abnormal arterial blood gases (ABGs)
Nursing Actions:
Maintain oxygen therapy as prescribed, position the patient for optimal ventilation, and monitor for signs of respiratory fatigue.
3. Renal System
The kidneys are sensitive to poor perfusion and toxins. Acute kidney injury (AKI) can develop quickly.
Signs to monitor:
- Decreased urine output (< 0.5 mL/kg/hr)
- Elevated BUN and creatinine
- Fluid retention or edema
Nursing Actions:
Measure intake and output (I&O) accurately, assess daily weights, and monitor for electrolyte imbalances.
4. Hepatic System
Liver dysfunction affects metabolism, detoxification, and coagulation.
Signs to monitor:
- Jaundice
- Elevated liver enzymes (ALT, AST)
- Coagulopathy (increased INR or bleeding)
- Altered mental status (hepatic encephalopathy)
Nursing Actions:
Monitor lab results closely, assess for bruising or bleeding, and report early signs of hepatic failure.
5. Neurological System
Changes in mental status are often one of the first indicators of hypoxia or organ dysfunction.
Signs to monitor:
- Confusion, agitation, or restlessness
- Decreased level of consciousness
- Pupillary changes
Nursing Actions:
Perform frequent neurological checks and assess the Glasgow Coma Scale (GCS) regularly.
6. Gastrointestinal System
Reduced perfusion can lead to ileus or stress ulcers.
Signs to monitor:
- Abdominal distention
- Decreased bowel sounds
- Occult blood in stool
Nursing Actions:
Monitor bowel function, prevent constipation, and maintain nutritional support as prescribed.
🧩 Nursing Priorities in Multi-Organ Failure
1. Continuous Monitoring:
Track vital signs, oxygen saturation, urine output, and neurological status every hour or more frequently if the patient is unstable.
2. Early Intervention:
Report subtle changes immediately — early detection saves lives.
3. Supportive Care:
Administer fluids, oxygen, medications, and nutrition according to the care plan.
4. Collaborate with the Healthcare Team:
Work closely with physicians, respiratory therapists, and pharmacists to ensure coordinated care.
5. Documentation:
Record all assessments, interventions, and patient responses accurately — a vital part of safe nursing practice.
💡 NCLEX Tips for Nurses
For the NCLEX, expect questions about:
- Early recognition of sepsis and MODS
- Prioritization of care in critical situations
- Fluid and electrolyte management
- Monitoring for organ-specific dysfunction
Remember: Early identification + prompt intervention = better outcomes.
📚 How Nursing Bundles Help
Comprehensive nursing bundles are designed to simplify complex topics like multi-organ failure for nursing students and RN nurses. These bundles combine pathophysiology, nursing interventions, NCLEX-style questions, and real-world case scenarios to enhance understanding and clinical readiness.
🩺 Key Takeaway for Registered Nurses
Multi-organ failure requires vigilant observation and timely nursing action. As a registered nurse, you play a central role in detecting subtle clinical changes and coordinating care that supports recovery. Through continuous monitoring and teamwork, nurses can make a lifesaving difference.
🩺 FAQ: Monitoring for Signs of Multi-Organ Failure
Multi-organ failure, also known as multiple organ dysfunction syndrome (MODS), occurs when two or more organ systems stop functioning properly due to severe illness, sepsis, or trauma. It’s a critical condition that requires intensive monitoring and immediate nursing interventions.
Early signs may include:
Low urine output
Decreased oxygen saturation
Hypotension or irregular heart rate
Altered mental status
Increased liver enzymes or abnormal lab results
Early recognition allows nurses and registered nurses (RN nurses) to intervene before the condition worsens.
Patients with sepsis, severe trauma, burns, pancreatitis, or prolonged hypotension are at greatest risk. A vigilant nurse must closely monitor these patients for any subtle signs of deterioration.
Monitor for increased respiratory effort, low SpO₂, and abnormal ABG results. Nurses should assess lung sounds frequently and report signs of respiratory distress immediately.
Key lab values include:
BUN and creatinine (renal function)
Liver enzymes (ALT, AST)
Electrolytes (especially potassium and sodium)
Arterial blood gases (ABGs)
Monitoring trends helps the registered nurse identify organ deterioration early.