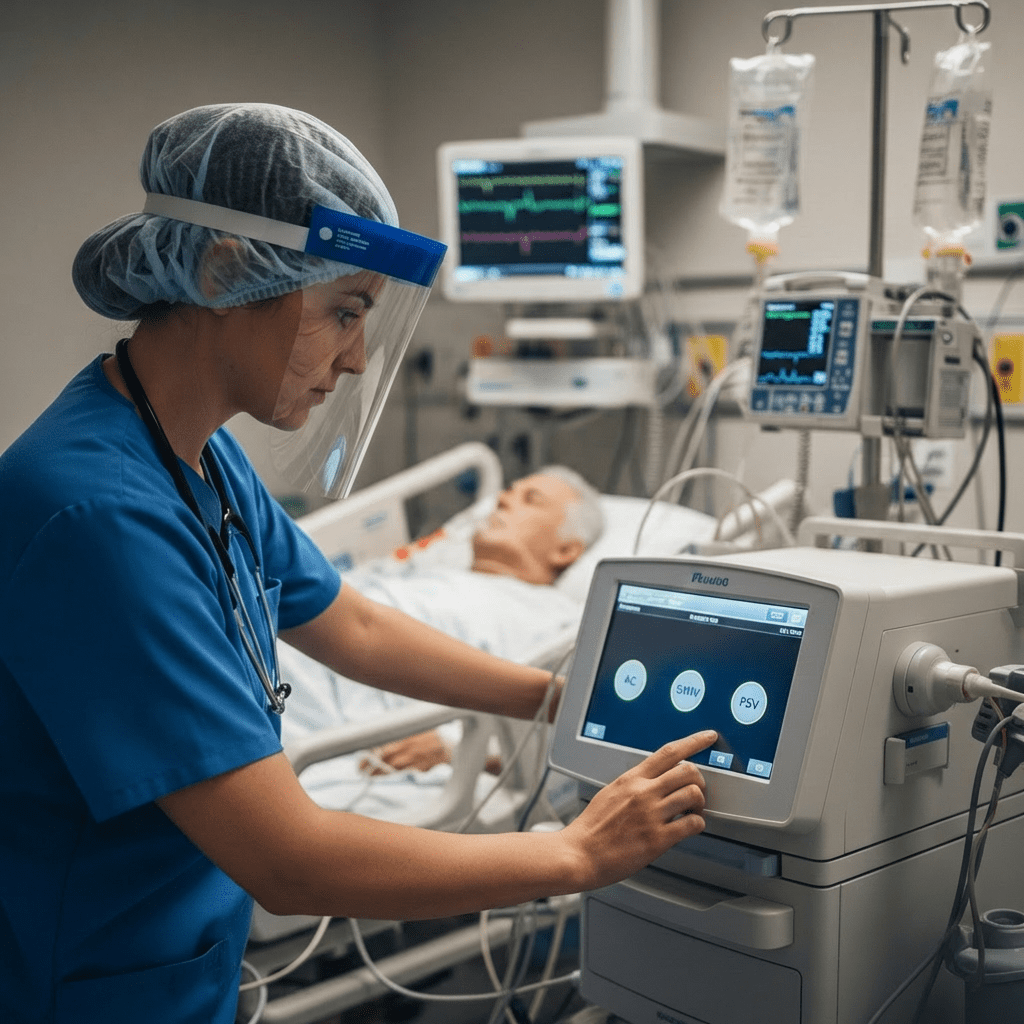
Mechanical ventilation is a life-saving intervention commonly used in critical care. For every ICU nurse, understanding ventilator modes such as Assist-Control (AC), Synchronized Intermittent Mandatory Ventilation (SIMV), and Pressure Support Ventilation (PSV) is essential for safe patient management. In addition, ventilator settings and interpretation are frequently tested on the NCLEX, making this topic crucial for both nursing students and registered nurses (RN nurses).
Because ventilator modes directly affect oxygenation, carbon dioxide removal, and patient comfort, nurses must not only recognize the differences but also understand their clinical implications.
Why Mechanical Ventilation Knowledge Matters in Nursing
Mechanical ventilation supports or replaces spontaneous breathing. However, inappropriate settings can cause complications such as barotrauma, volutrauma, or respiratory acidosis.
Therefore, the registered nurse plays a key role in:
- Monitoring respiratory status
- Assessing patient-ventilator synchrony
- Preventing ventilator-associated complications
- Communicating changes promptly
For NCLEX preparation, ventilator questions often test understanding of mode differences, alarm troubleshooting, and appropriate nursing interventions.
Assist-Control (AC) Ventilation
What Is Assist-Control?
Assist-Control (AC) ventilation delivers a preset tidal volume or pressure with every breath. The ventilator provides a full mandatory breath whether triggered by the patient or by the machine.
In simple terms:
Every breath is fully supported.
Clinical Indications
AC mode is commonly used for:
- Severe respiratory failure
- Acute Respiratory Distress Syndrome (ARDS)
- Patients who are heavily sedated
- Patients with minimal spontaneous effort
Nursing Implications of AC Mode
Because every breath delivers a full tidal volume, patients may hyperventilate if they trigger rapid breaths. This can lead to respiratory alkalosis.
Therefore, the ICU nurse must monitor:
- Respiratory rate
- Arterial blood gases (ABGs)
- Patient comfort
- Signs of air trapping
Additionally, high tidal volumes increase the risk of lung injury. Lung-protective strategies are often included in critical care nursing bundles to prevent ventilator-associated complications.
NCLEX Tip for AC Mode
If a patient is breathing rapidly on AC and ABGs show alkalosis, the nurse should anticipate adjustments to respiratory rate or sedation levels.
Synchronized Intermittent Mandatory Ventilation (SIMV)
What Is SIMV?
SIMV delivers a set number of mandatory breaths. However, between those breaths, the patient can breathe spontaneously.
Unlike AC mode:
Not every breath is fully supported.
Clinical Indications
SIMV is often used for:
- Weaning patients off the ventilator
- Patients with partial respiratory drive
- Gradual transition to spontaneous breathing
Nursing Implications of SIMV
Because spontaneous breaths may not receive full support, patients can become fatigued.
The RN nurse must monitor:
- Signs of respiratory distress
- Increased work of breathing
- Accessory muscle use
- Decreasing oxygen saturation
Moreover, if spontaneous breaths are insufficient, carbon dioxide levels may rise, leading to respiratory acidosis.
In many ICU nursing bundles, weaning protocols are standardized to reduce complications.
NCLEX Tip for SIMV
If a patient on SIMV develops fatigue and rising CO₂ levels, the nurse should recognize inadequate spontaneous ventilation and notify the provider.
Pressure Support Ventilation (PSV)
What Is PSV?
Pressure Support Ventilation provides a preset pressure to assist spontaneous breaths. However, the patient initiates all breaths.
In other words:
The ventilator supports effort but does not control breathing.
Clinical Indications
PSV is commonly used during:
- Weaning trials
- Spontaneous breathing trials (SBTs)
- Mild respiratory weakness
Nursing Implications of PSV
Since PSV depends entirely on patient effort, it is unsuitable for patients who are apneic or heavily sedated.
The registered nurse should assess:
- Respiratory rate trends
- Tidal volume consistency
- Oxygenation status
- Signs of fatigue
If the patient becomes exhausted, respiratory failure can occur quickly.
NCLEX Tip for PSV
If a patient becomes lethargic with shallow respirations on PSV, the nurse must recognize impending respiratory failure and intervene immediately.
Comparing AC, SIMV, and PSV
| Mode | Who Initiates Breath | Who Controls Volume | Best For |
|---|---|---|---|
| AC | Patient or Ventilator | Ventilator | Full support |
| SIMV | Mixed | Ventilator (mandatory only) | Weaning |
| PSV | Patient | Patient (pressure assisted) | Spontaneous breathing |
Understanding these differences is essential for both clinical nursing and NCLEX success.
Common Ventilator Alarms and Nursing Actions
Mechanical ventilation requires constant monitoring. Therefore, nurses must respond quickly to alarms.
Common alarms include:
High Pressure Alarm:
- Kinked tubing
- Secretions
- Patient coughing
Low Pressure Alarm:
- Disconnection
- Leak in circuit
In every scenario, patient assessment comes first. On the NCLEX, the correct answer almost always prioritizes checking the patient before adjusting equipment.
Preventing Ventilator-Associated Complications
Mechanical ventilation increases the risk of complications such as:
- Ventilator-Associated Pneumonia (VAP)
- Barotrauma
- Oxygen toxicity
A structured nursing bundle often includes:
- Head-of-bed elevation
- Daily sedation interruption
- Oral care with chlorhexidine
- Spontaneous breathing trials
These evidence-based interventions improve patient outcomes and are frequently emphasized in critical care nursing education.
The Role of the Registered Nurse in Mechanical Ventilation
The RN nurse plays a central role in ventilator management by:
- Monitoring ABGs
- Assessing lung sounds
- Ensuring appropriate sedation
- Coordinating with respiratory therapy
- Documenting ventilator changes accurately
Additionally, clear documentation protects the registered nurse legally and ensures continuity of care.
NCLEX High-Yield Ventilator Concepts
For exam preparation, remember:
- AC = full support
- SIMV = partial support
- PSV = patient-driven
Furthermore, always prioritize:
- Airway
- Breathing
- Oxygenation
Many ventilator questions test prioritization and recognition of respiratory distress.
Final Clinical Pearls for Nurses
- Monitor trends, not just single values
- Always assess the patient before adjusting settings
- Watch for respiratory fatigue during weaning
- Collaborate with respiratory therapy
- Follow your unit’s mechanical ventilation nursing bundle
By understanding ventilator modes clinically rather than memorizing definitions, nurses can improve patient safety and build confidence for the NCLEX.
Conclusion
Mechanical ventilation modes such as AC, SIMV, and PSV are essential concepts in critical care nursing. Each mode serves a specific purpose, and selecting the appropriate one depends on patient condition and respiratory status.
For every nurse and registered nurse working in ICU settings, mastering ventilator interpretation is vital for safe practice. Moreover, since ventilator management is frequently tested on the NCLEX, consistent review and structured learning through a comprehensive nursing bundle can greatly enhance both exam performance and bedside competence.