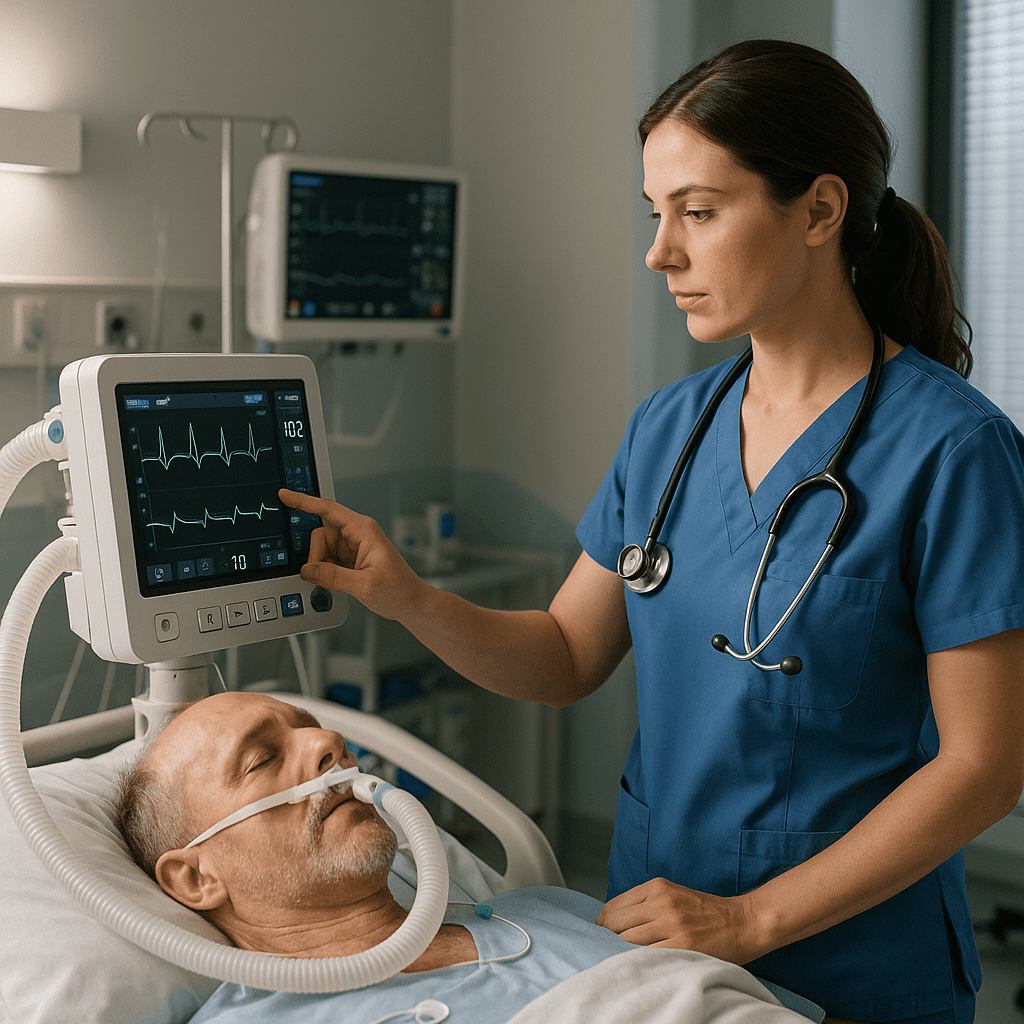
Mechanical ventilation is a life-saving intervention used to support patients who cannot maintain adequate ventilation on their own. For every nurse, understanding ventilator management is essential—not only for ensuring patient safety but also for NCLEX success. Whether you are a registered nurse (RN) or a nursing student preparing for exams, mastering the principles of ventilator care is part of advanced nursing practice and critical care competency.
🩺 What Is Mechanical Ventilation?
Mechanical ventilation delivers oxygen and removes carbon dioxide through an artificial airway—either an endotracheal tube (ETT) or tracheostomy. It can be used for patients with respiratory failure, ARDS, trauma, or postoperative complications. For a nurse, knowing how to monitor and manage these patients is vital to prevent complications and optimize outcomes.
💨 Key Nursing Responsibilities for Ventilated Patients
1. Maintain Airway Patency
Ensure the airway is clear and secured. Check the endotracheal tube (ETT) position and cuff pressure regularly to prevent air leaks and aspiration.
2. Monitor Ventilator Settings
Understand basic parameters such as:
- Tidal volume (VT): Amount of air delivered per breath
- FiO₂: Fraction of inspired oxygen
- PEEP: Positive end-expiratory pressure to prevent alveolar collapse
- Rate: Number of breaths delivered per minute
A registered nurse should monitor these values and collaborate with the respiratory therapist to ensure optimal ventilation support.
3. Assess Patient-Ventilator Synchrony
Observe for signs of discomfort, agitation, or asynchronous breathing. If present, check the ventilator settings or sedation level.
4. Prevent Ventilator-Associated Pneumonia (VAP)
Follow the nursing bundle for VAP prevention:
- Elevate the head of bed (30–45°)
- Provide oral care with chlorhexidine
- Perform daily sedation breaks and assess readiness to extubate
- Use sterile suctioning techniques
⚠️ Recognizing Complications
Barotrauma — from excessive pressure causing lung injury
Hypoxia or hyperoxia — from incorrect FiO₂ or malfunctioning equipment
Hypotension — due to increased intrathoracic pressure
Infection — especially ventilator-associated pneumonia (VAP)
Nurses must continuously monitor oxygen saturation, breath sounds, ABG results, and patient behavior to identify these early.
🧠 NCLEX Tips for Nurses
On the NCLEX, mechanical ventilation questions often test your knowledge of:
- Prioritization (ABCs)
- Recognizing ventilator alarms
- Preventing complications like VAP
- Identifying early signs of hypoxia
Quick reminders for RNs:
- High-pressure alarm: May indicate obstruction, coughing, or kinked tubing.
- Low-pressure alarm: Could mean a disconnection or cuff leak.
- Always assess the patient first—not just the machine.
💬 Patient and Family Education
As part of holistic nursing care, explain procedures clearly to the patient (if conscious) and family. Use simple terms to describe the ventilator’s purpose and reassure them that it’s a temporary support system.
🧩 Documentation and Communication
Accurate documentation includes ventilator settings, patient tolerance, secretions, oxygen saturation, and any interventions performed. Effective handoffs between nurses during shift changes ensure patient safety and continuity of care.
🩹 The Role of the Registered Nurse in Mechanical Ventilation
Every registered nurse plays a crucial role in maintaining airway security, preventing infection, managing sedation, and collaborating with physicians and respiratory therapists. This teamwork is fundamental for patient recovery and aligns with evidence-based nursing bundles designed to improve outcomes in critical care.
🧾 Key Takeaway for NCLEX and Clinical Practice
Mechanical ventilation requires continuous vigilance, accurate assessment, and proactive nursing interventions. As a nurse or RN, understanding ventilator parameters, responding to alarms promptly, and applying preventive care bundles will not only enhance patient outcomes but also strengthen your NCLEX readiness.
🌟 Final Thought
Mechanical ventilation management is one of the most advanced yet rewarding aspects of nursing practice. Through diligent observation, patient education, and adherence to evidence-based nursing bundles, registered nurses ensure safe, compassionate, and effective care for critically ill patients.
❓ FAQ: Managing Patients on Mechanical Ventilation
The nurse’s primary responsibility is to ensure airway patency, monitor ventilator settings, assess patient response, and prevent complications such as ventilator-associated pneumonia (VAP). Continuous assessment of oxygenation, respiratory rate, and vital signs is essential.
Nurses should follow the VAP prevention nursing bundle, which includes elevating the head of the bed, providing regular oral care, using sterile suctioning techniques, and assessing readiness for extubation daily. Strict hand hygiene is also a must.
Always assess the patient first, not the machine. High-pressure alarms may indicate obstruction or coughing, while low-pressure alarms can signal disconnection or cuff leaks. Quickly identify and correct the cause to prevent respiratory compromise.