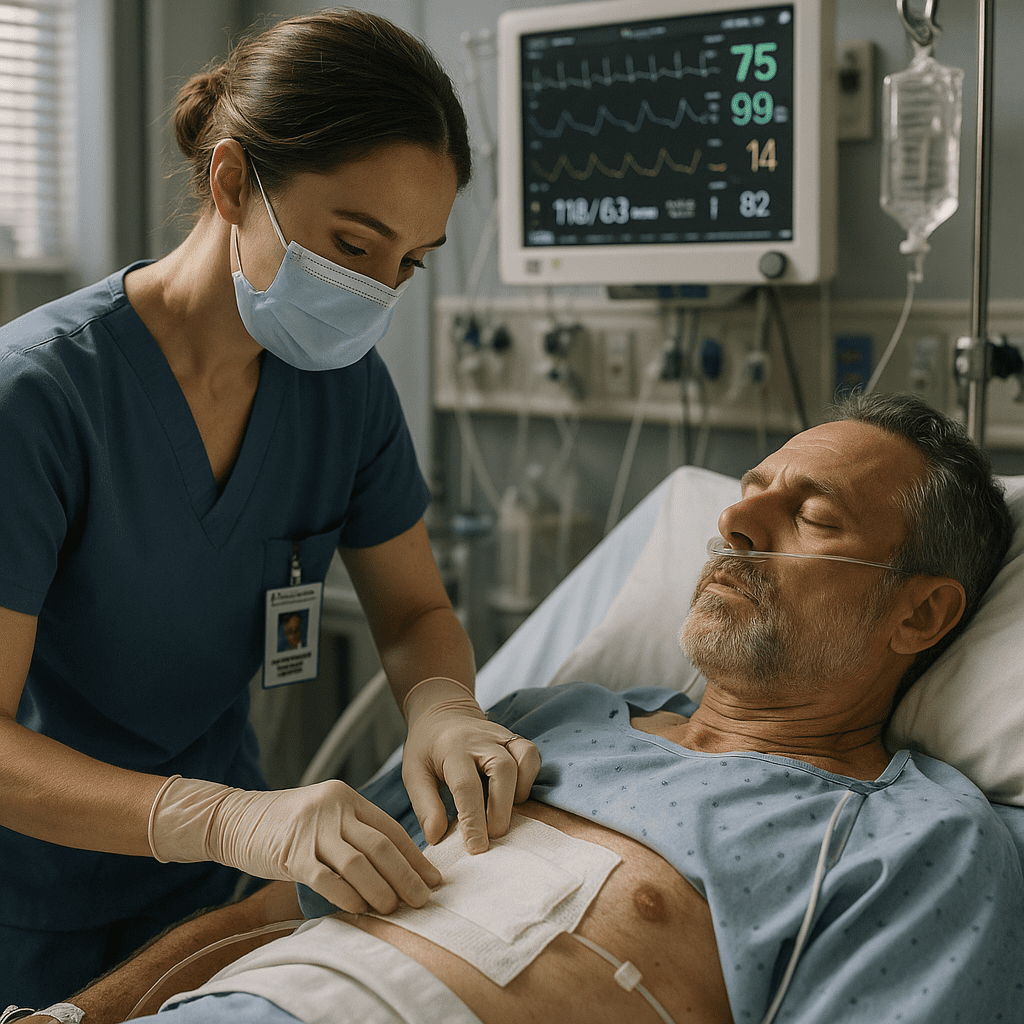
Managing postoperative complications is a critical responsibility for every registered nurse (RN). After surgery, patients are at risk for issues like bleeding, infection, respiratory distress, electrolyte imbalances, and impaired wound healing. Understanding how to identify and respond to these complications is essential not only for safe patient care but also for NCLEX success, as postoperative scenarios appear frequently in exam questions.
This guide breaks down the most important postoperative complications and the nursing actions required to keep patients safe.
🩺 Why Postoperative Management Matters in Nursing
After surgery, the body undergoes major stress, and complications can develop rapidly. A nurse must continuously assess, intervene, and communicate early warning signs. Effective postoperative care also reflects evidence-based nursing bundle practices that support patient safety and recovery.
Because postoperative assessment is a core topic on the NCLEX, every RN nurse and nursing student should master these skills.
✅ Common Postoperative Complications and How Nurses Manage Them
1. Postoperative Hemorrhage (Bleeding)
Bleeding can occur immediately after surgery or within several hours.
Nursing Assessment
- Drop in blood pressure
- Increased heart rate
- Cool, clammy skin
- Swelling or increased drainage from incision site
- Low hemoglobin/hematocrit
Nursing Actions
- Apply pressure to the site if visible
- Notify the surgical team immediately
- Prepare the patient for possible return to OR
- Monitor vital signs every 5–15 minutes
- Ensure IV access and fluids are running
📌 NCLEX Tip: If a surgical dressing is soaked, reinforce once, then notify the provider. Do not remove the dressing.
2. Infection (Surgical Site Infection & Systemic Infection)
Infections can appear days after surgery, but early signs may develop in the first 24–48 hours.
Nursing Assessment
- Redness, heat, or swelling around incision
- Purulent drainage
- Fever or chills
- Elevated WBC count
Nursing Actions
- Perform hand hygiene and maintain sterile technique
- Educate the patient on incision care
- Administer antibiotics as ordered
- Monitor temperature regularly
- Document changes in wound appearance
📌 NCLEX Tip: For infection prevention, the priority nursing action is hand hygiene before wound care.
3. Respiratory Complications (Atelectasis, Pneumonia)
Immobility, pain, and sedation all increase risk.
Nursing Assessment
- Shortness of breath
- Low oxygen saturation
- Diminished lung sounds
- Fever (with pneumonia)
Nursing Actions
- Encourage incentive spirometer use every hour
- Teach deep breathing and coughing
- Reposition the patient every 1–2 hours
- Provide pain control to encourage mobility
- Elevate HOB to 30–45°
📌 NCLEX Tip: Atelectasis is the most common early postoperative complication.
4. Deep Vein Thrombosis (DVT)
Surgical patients are at high risk due to immobility.
Nursing Assessment
- Swelling or warmth in one leg
- Calf tenderness
- Redness
Nursing Actions
- Apply compression stockings or SCDs
- Administer anticoagulants as ordered
- Encourage early ambulation
- Avoid massaging the legs
📌 NCLEX Tip: If a DVT is suspected, put the patient on bed rest and notify the provider.
5. Fluid & Electrolyte Imbalances
Fluid shifts and blood loss can lead to dehydration, overload, or electrolyte disorders.
Nursing Assessment
- Confusion, irritability
- Weakness or arrhythmias
- Low urine output
- Abnormal electrolytes (Na, K, Mg, Ca)
Nursing Actions
- Monitor I&O strictly
- Assess daily weights
- Replace fluids or electrolytes within prescribed range
- Watch for arrhythmias on cardiac monitoring
📌 NCLEX Tip: Potassium imbalance is especially important—high or low levels can cause life-threatening dysrhythmias.
6. Nausea, Vomiting & Aspiration Risk
Common after anesthesia.
Nursing Assessment
- Nausea or retching
- Hypoactive bowel sounds
- Delayed gastric emptying
Nursing Actions
- Administer antiemetics
- Position in side-lying to prevent aspiration
- Advance diet slowly from clear liquids
- Assess bowel function
7. Impaired Wound Healing
Healing may be delayed in older adults, diabetics, and immunocompromised patients.
Nursing Assessment
- Wound dehiscence (opening of incision)
- Evisceration (organs protruding)
- Slow granulation
Nursing Actions
- Cover with sterile, moist saline dressing
- Keep patient NPO
- Call provider immediately
- Do NOT push organs back in
📌 NCLEX Tip: Evisceration is an emergency—cover with a sterile saline dressing and prepare for surgery.
✅ Key NCLEX Takeaways for Postoperative Nursing Care
- The first priority is always airway, breathing, circulation (ABCs).
- Look for early signs of deterioration—tachycardia often comes before hypotension.
- The nurse must report abnormal findings immediately and act quickly.
- Monitor vital signs frequently—every 15 minutes in the immediate postop stage.
- Use evidence-based nursing bundles to reduce complications like pneumonia, infection, and DVT.
These principles help both the registered nurse and any nursing student stay prepared for real-world scenarios and NCLEX questions.
✅ Final Thoughts
Managing postoperative complications requires vigilance, rapid assessment, and strong critical-thinking skills. Every RN nurse plays a vital role in ensuring a safe recovery by monitoring for early warning signs, providing education, and implementing interventions from evidence-based nursing practices. Mastering this topic greatly strengthens clinical confidence and boosts NCLEX readiness.