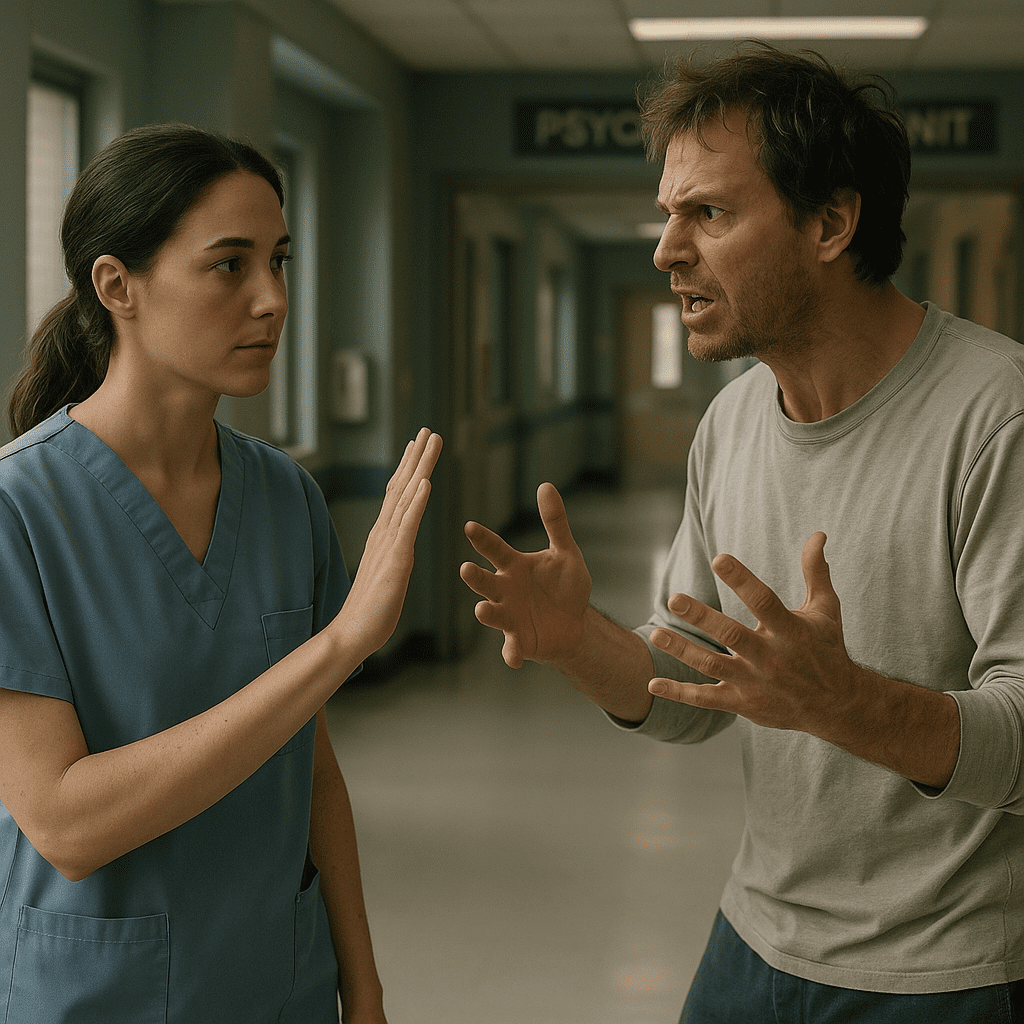
Aggressive behavior is a challenge many nurses face in clinical settings—from emergency departments to psychiatric units and long-term care facilities. For an RN nurse or registered nurse, knowing how to respond safely protects both the patient and the healthcare team. This topic is also highly tested on the NCLEX, making it essential for students and professionals using any nursing bundle or study materials.
This guide explains the causes, risk factors, de-escalation strategies, and safety interventions every nursing professional should master.
What Causes Aggressive Behavior?
Aggression can be verbal, emotional, or physical. Understanding the cause helps the nurse choose the safest intervention.
Common Causes
- Psychiatric disorders (schizophrenia, bipolar disorder, personality disorders)
- Substance intoxication or withdrawal
- Medical conditions (hypoxia, infections, dementia)
- Pain or frustration
- Fear, anxiety, or overstimulation
On the NCLEX, the priority is always safety—never ignore early warning signs of escalation.
Early Warning Signs
Registered nurses must identify cues that aggression may be building:
- Clenched fists, pacing
- Raised voice, rapid speech
- Hostile or threatening statements
- Restlessness or agitation
- Staring or glaring
- Sudden quietness after agitation (a danger sign)
RN nurses should intervene early, before behavior becomes violent.
Nursing Interventions: How to Respond Safely
1. Use De-Escalation Techniques First
De-escalation is an essential nursing skill tested on the NCLEX.
- Stay calm and speak softly
- Maintain a non-threatening stance
- Keep a safe distance
- Set clear, respectful limits
- Offer choices (enhances patient control)
- Remove triggers (noise, crowding, stimulation)
Example:
“Mr. A, I want to help. Let’s talk in a quieter room.”
2. Prioritize Safety
For the RN nurse, safety always comes before therapeutic communication.
- Ensure an exit is accessible at all times
- Keep dangerous objects out of reach
- Do not turn your back on an escalating patient
- Call for help early—do not manage aggression alone
3. Consider Pharmacologic Interventions
If de-escalation fails:
- Antipsychotics: Haloperidol, Olanzapine
- Benzodiazepines: Lorazepam
Administer only per protocol and monitor for side effects.
This topic appears throughout NCLEX nursing psychiatric sections.
4. Physical Restraints (Last Resort)
Use only when:
- The patient poses immediate danger
- Other interventions have failed
Key nursing responsibilities:
- Get a provider order
- Use least restrictive restraint
- Assess circulation, breathing, and skin every 15 minutes
- Document thoroughly
Nursing Care After an Aggressive Episode
Reflection and follow-up care are vital for both patient and staff.
- Debrief with the patient
- Identify triggers together
- Evaluate what interventions worked
- Update the care plan
- Provide emotional support to staff involved
- Document objectively (essential for NCLEX legal/ethical questions)
Education for Patients and Families
A registered nurse should teach families how to support individuals at risk of aggression:
- Identify triggers
- Create structured routines
- Promote medication adherence
- Encourage coping strategies
- Use simple communication
- Avoid arguing when the person is escalated
Key NCLEX Tips
- Never use restraints as punishment
- Safety for staff and patient is always the priority
- Early de-escalation prevents violence
- RN nurses must use therapeutic communication
- Document behavior, not subjective interpretation
FAQ: Managing Aggressive Behavior Safely
Use de-escalation techniques—stay calm, maintain distance, and speak softly. This is the first-line NCLEX-priority action.
Only when the patient is a danger to themselves or others, and all other interventions have failed.
Common options include haloperidol, olanzapine, and lorazepam, depending on the patient’s condition.
Frequent monitoring, documentation, and ensuring restraints are the least restrictive option.