Magnesium is often overlooked compared to potassium and calcium, yet it plays a critical role in maintaining cardiac electrical stability. For every nurse, especially the ICU registered nurse (RN nurse), understanding magnesium’s impact on the heart is essential for preventing life-threatening arrhythmias. Because electrolyte imbalances and ECG interpretation are heavily tested on the NCLEX, mastering magnesium physiology strengthens both exam preparation and advanced nursing practice.
Magnesium is not just a “minor electrolyte” — it is a stabilizer of cardiac rhythm.
Normal Magnesium Levels and Distribution
Normal serum magnesium:
1.7–2.2 mg/dL
Magnesium is primarily intracellular and functions as:
- A cofactor in over 300 enzymatic reactions
- A regulator of sodium-potassium ATPase
- A modulator of calcium channels
- A stabilizer of myocardial cell membranes
For the RN nurse, recognizing magnesium’s influence on cardiac excitability is crucial in critical care.
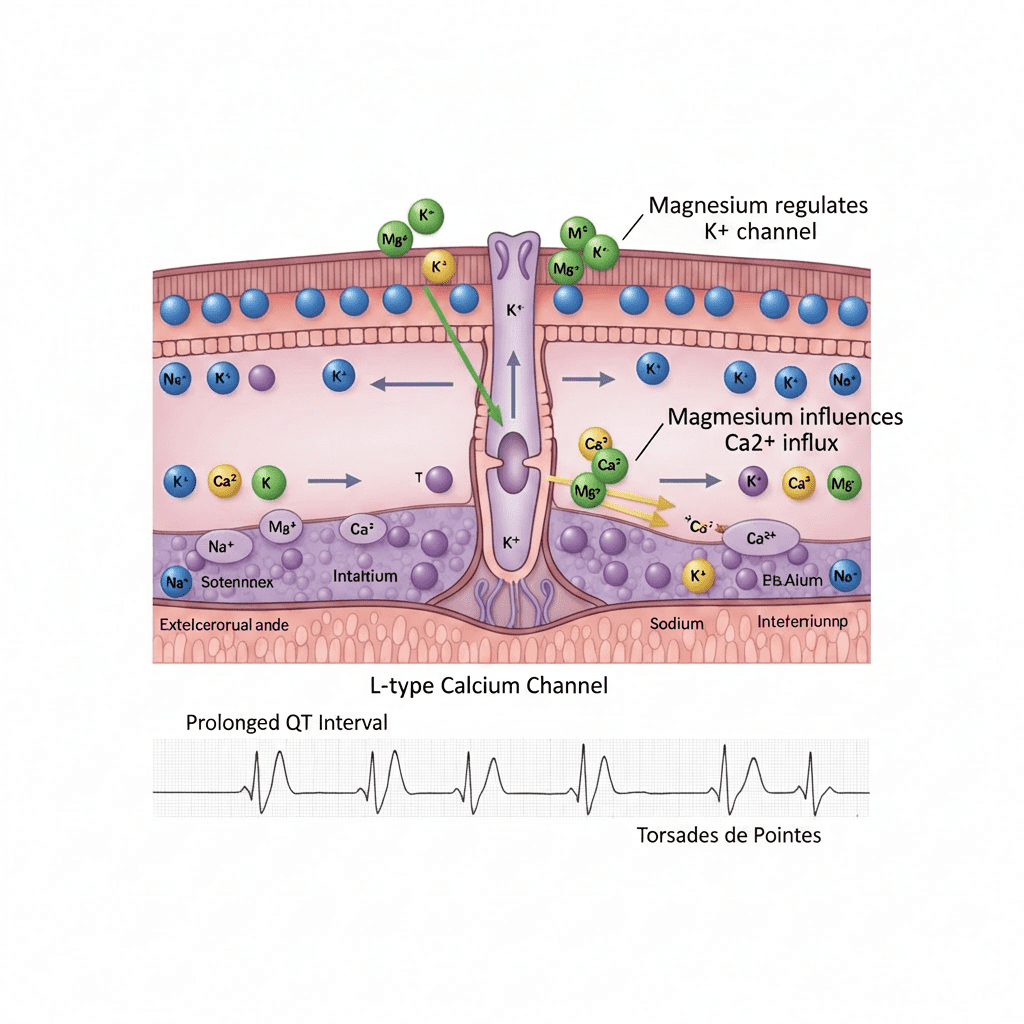
Magnesium and the Cardiac Action Potential
Cardiac electrical activity depends on precise ion movement:
- Sodium (Na⁺) → depolarization
- Calcium (Ca²⁺) → plateau phase
- Potassium (K⁺) → repolarization
Magnesium regulates all three.
Magnesium stabilizes cardiac cells by regulating potassium movement and controlling calcium influx.
Without adequate magnesium:
- Potassium cannot remain inside cells effectively
- Calcium influx increases
- Cardiac cells become hyperexcitable
This increases arrhythmia risk.
Magnesium and the Sodium-Potassium Pump
Magnesium activates the Na⁺/K⁺ ATPase pump.
This pump:
- Moves potassium into cells
- Moves sodium out of cells
- Maintains resting membrane potential
Low magnesium impairs this pump, leading to:
- Hypokalemia that is resistant to correction
- Increased arrhythmia risk
The registered nurse must check magnesium levels when potassium replacement is ineffective.
Hypomagnesemia and Cardiac Instability
Hypomagnesemia (<1.7 mg/dL) can cause:
- Prolonged QT interval
- Torsades de Pointes
- Ventricular arrhythmias
- Atrial fibrillation
- PVCs
On the NCLEX, Torsades de Pointes is classically treated with IV magnesium.
Even if magnesium level is normal, magnesium sulfate may still be administered for Torsades.
Why Hypomagnesemia Causes Arrhythmias
When magnesium is low:
- Calcium channels remain overly active
- Potassium loss increases
- Cardiac cells depolarize more easily
This creates electrical instability.
The RN nurse must monitor telemetry closely in patients with:
- Alcohol use disorder
- Diuretic therapy
- Malnutrition
- GI losses
Hypermagnesemia and Cardiac Effects
Hypermagnesemia (>2.5 mg/dL) is less common but dangerous.
Causes include:
- Renal failure
- Excess magnesium administration
- Antacid or laxative overuse
Cardiac effects:
- Bradycardia
- Hypotension
- Heart block
- Cardiac arrest (severe cases)
The nurse must assess deep tendon reflexes, as loss of reflexes is an early sign.
Magnesium and Torsades de Pointes
Torsades is a polymorphic ventricular tachycardia associated with prolonged QT.
Magnesium sulfate works by:
- Stabilizing myocardial membranes
- Reducing calcium influx
- Shortening QT interval
This is a high-yield NCLEX concept.
If a patient develops Torsades, the RN nurse should anticipate IV magnesium administration immediately.
Magnesium’s Relationship with Potassium and Calcium
Electrolytes work together.
Low magnesium often coexists with:
- Hypokalemia
- Hypocalcemia
Magnesium deficiency reduces parathyroid hormone (PTH) release, contributing to hypocalcemia.
A structured nursing bundle for electrolyte management should include:
- Monitoring magnesium
- Monitoring potassium
- Monitoring calcium
- Continuous ECG monitoring
Correcting magnesium often corrects potassium.
ECG Changes Associated with Magnesium Imbalances
Hypomagnesemia
- Prolonged QT
- Ventricular arrhythmias
- Torsades
Hypermagnesemia
- Prolonged PR interval
- Widened QRS
- Bradycardia
The registered nurse must correlate lab values with ECG findings.
Magnesium in Acute Coronary Syndromes
Magnesium may:
- Reduce ventricular arrhythmias
- Improve myocardial stability
- Decrease sudden cardiac death risk
Although not routinely given for all cardiac patients, magnesium is critical in arrhythmia management.
IV Magnesium Administration: Nursing Considerations
The RN nurse must:
- Administer IV magnesium slowly
- Monitor blood pressure
- Monitor respiratory rate
- Assess reflexes
- Monitor cardiac rhythm
Rapid infusion can cause hypotension and flushing.
Magnesium should never be given as a rapid IV push unless during cardiac arrest per protocol.
This is commonly tested on the NCLEX.
Magnesium and Renal Function
Magnesium is excreted by the kidneys.
Patients with renal failure are at higher risk for hypermagnesemia.
The registered nurse must:
- Monitor creatinine
- Adjust dosing as needed
- Assess for toxicity
Nursing Bundle for Cardiac Electrical Stability
A cardiac electrolyte nursing bundle may include:
- Continuous telemetry
- Daily magnesium levels in ICU patients
- Monitoring potassium and calcium
- Prompt replacement of deficiencies
- Renal function monitoring
- Documentation of ECG changes
Consistency improves patient safety.
NCLEX High-Yield Magnesium Review
- Normal magnesium: 1.7–2.2 mg/dL
- Low magnesium → prolonged QT → Torsades
- Treat Torsades with IV magnesium
- Magnesium stabilizes potassium
- Monitor reflexes in hypermagnesemia
- Renal failure increases magnesium toxicity risk
If potassium is not correcting despite replacement, check magnesium.
Integrating Magnesium Knowledge into Nursing Practice
Understanding magnesium’s role in cardiac electrical stability allows the experienced RN nurse to anticipate complications before they become emergencies.
By applying a structured nursing bundle, nurses can:
- Prevent ventricular arrhythmias
- Reduce cardiac arrest risk
- Improve telemetry interpretation
- Strengthen critical thinking
This advanced understanding also enhances NCLEX performance.
Final Thoughts
Magnesium is a powerful regulator of cardiac electrical stability. For every nurse and registered nurse, mastering magnesium physiology is essential for safe and effective nursing care.
Because electrolyte imbalances and arrhythmias are heavily emphasized on the NCLEX, understanding magnesium’s role in stabilizing myocardial cells strengthens both exam readiness and bedside confidence.
In critical care nursing, sometimes the most overlooked electrolyte is the one that protects the heart the most.