Every registered nurse (RN) must be able to recognize the early signs of ischemia and myocardial infarction (MI) — both on the ECG and through clinical assessment. Prompt recognition can mean the difference between life and death.
For NCLEX candidates, this topic is a frequent focus area in cardiovascular nursing questions. This comprehensive nursing guide breaks down ECG patterns, nursing priorities, and interventions related to ischemia and myocardial infarction to help both students and clinical nurses strengthen their practice.
❤️ 1. Understanding Ischemia and Myocardial Infarction
What Is Ischemia?
Myocardial ischemia occurs when blood flow to the heart muscle is reduced, often due to partial obstruction of the coronary arteries. This leads to oxygen deprivation and reversible cellular injury.
What Is Myocardial Infarction (MI)?
Myocardial infarction, or heart attack, results from complete blockage of blood flow, leading to irreversible myocardial cell death. Nurses must understand how ischemia progresses to injury and infarction for rapid intervention.
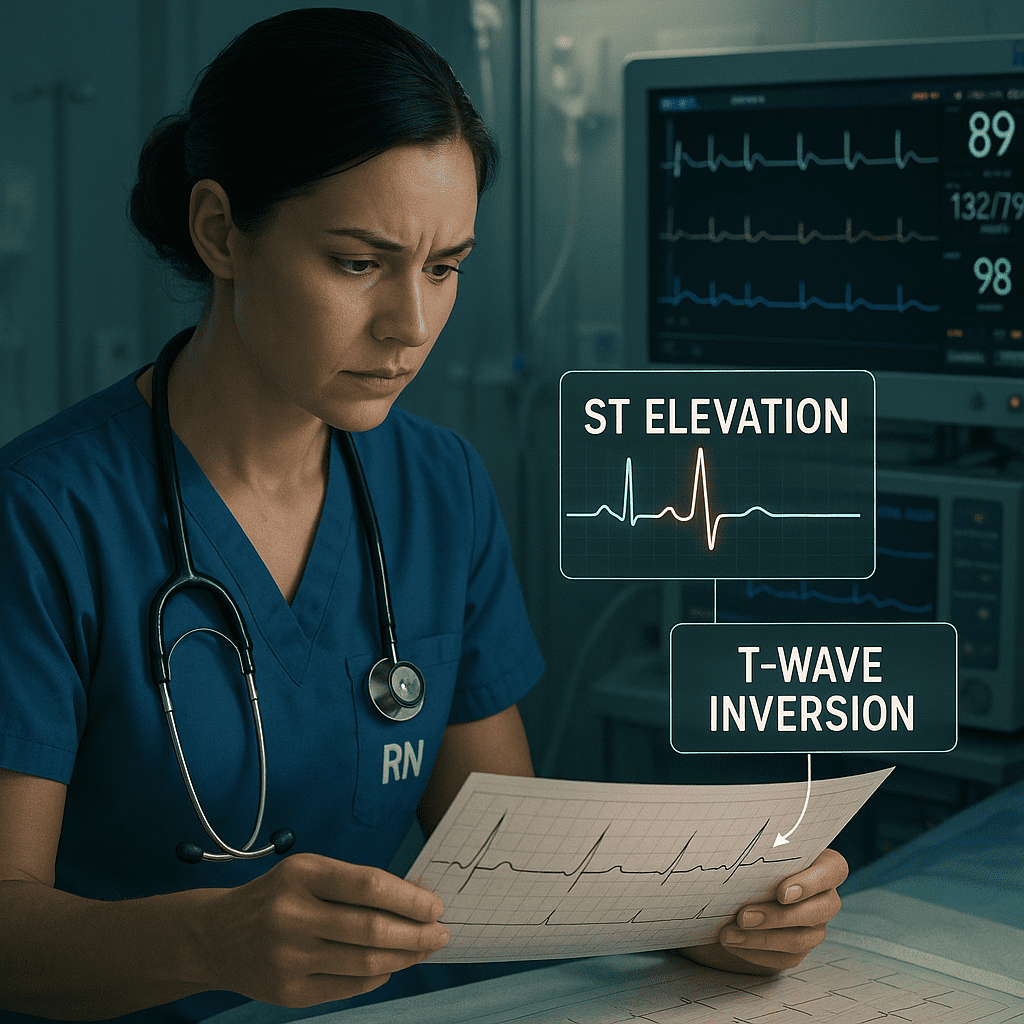
🩺 2. ECG Changes in Ischemia, Injury, and Infarction
Recognizing ECG changes is essential for registered nurses in telemetry, critical care, or emergency units — and a key concept in NCLEX cardiac questions.
| Stage | ECG Findings | Clinical Meaning |
|---|---|---|
| Ischemia | T-wave inversion or ST depression | Lack of oxygen; reversible |
| Injury | ST elevation (acute phase) | Ongoing damage; needs immediate reperfusion |
| Infarction | Pathological Q waves | Necrosis; irreversible damage |
NCLEX Tip:
Think of “I I I” → Ischemia = Inverted T, Injury = ST elevation, Infarction = Q waves.
💡 3. Localizing MI on the ECG
Understanding which leads correspond to specific heart regions is vital for accurate interpretation and appropriate nursing intervention.
| Region Affected | ECG Leads | Coronary Artery Involved |
|---|---|---|
| Anterior wall MI | V1–V4 | Left anterior descending (LAD) artery |
| Inferior wall MI | II, III, aVF | Right coronary artery (RCA) |
| Lateral wall MI | I, aVL, V5–V6 | Circumflex artery |
| Posterior wall MI | V7–V9 (posterior leads) | RCA or circumflex artery |
Nursing note: Always document which leads show abnormalities — it helps the care team localize the infarct and determine treatment urgency.
⚕️ 4. Nursing Priorities in Ischemia and Myocardial Infarction
Registered nurses play a vital role in both early recognition and post-MI management.
Key nursing actions include:
A. Early Recognition
- Assess chest pain (location, duration, character, radiation).
- Monitor for associated symptoms — shortness of breath, diaphoresis, nausea, anxiety.
- Obtain 12-lead ECG immediately.
- Measure troponin and CK-MB levels.
B. Acute Nursing Interventions (MONA mnemonic)
- M – Morphine: Relieves pain, reduces cardiac workload.
- O – Oxygen: Maintain saturation >94%.
- N – Nitrates: Dilate coronary vessels, relieve ischemia.
- A – Aspirin: Prevents platelet aggregation.
C. Ongoing Monitoring
- Continuous cardiac rhythm monitoring
- Watch for arrhythmias, heart failure, or cardiogenic shock
- Maintain IV access and vital signs every 5 minutes during the acute phase
🧠 5. NCLEX Nursing Focus
For NCLEX success, remember these key test points:
✅ ST elevation = emergency → call rapid response and prepare for PCI (percutaneous coronary intervention).
✅ Q waves indicate old MI, not current ischemia.
✅ Prioritize oxygen, aspirin, and ECG monitoring before invasive interventions.
✅ Evaluate response to nitroglycerin to differentiate cardiac vs. non-cardiac pain.
💬 6. Patient Education and Long-Term Nursing Care
Registered nurses must educate post-MI patients on:
- Medication adherence: Beta-blockers, ACE inhibitors, statins, and aspirin
- Lifestyle changes: Low-sodium diet, exercise, smoking cessation
- Warning signs: Chest discomfort, shortness of breath, fatigue
- Emotional support: Address depression and anxiety related to cardiac events
Nursing bundle care plans for MI patients often include psychosocial support, discharge teaching, and scheduled follow-up visits.
⚡ 7. Common Complications to Watch For
- Ventricular arrhythmias (VT/VF)
- Cardiogenic shock
- Pericarditis
- Heart failure
- Recurrent ischemia
Continuous ECG monitoring helps detect changes early — a core nursing responsibility.
Conclusion
For every nurse, recognizing ischemia and myocardial infarction patterns is a fundamental skill that combines critical thinking and clinical assessment.
Whether preparing for the NCLEX or working at the bedside, knowing how to interpret ECG changes, initiate prompt treatment, and provide patient-centered education is essential for improving outcomes.
By mastering these patterns, every RN nurse strengthens their ability to save lives — making cardiac care both precise and compassionate.
FAQ
T-wave inversion or ST depression, indicating reduced oxygen supply to the myocardium.
It signals myocardial injury — the heart muscle is actively being damaged and requires urgent intervention.
They represent irreversible myocardial necrosis, a hallmark of previous infarction.
The right coronary artery (RCA).
Apply MONA (Morphine, Oxygen, Nitrates, Aspirin), obtain ECG, and monitor vital signs continuously.