Intracranial pressure (ICP) monitoring is a cornerstone of Neuro ICU care. For every nurse, especially the critical care registered nurse (RN nurse), understanding ICP waveforms is essential for early detection of neurological deterioration. Because neuro assessment and increased ICP management are frequently tested on the NCLEX, mastering waveform interpretation strengthens both clinical judgment and exam performance.
In the Neuro ICU, subtle waveform changes can signal impending brain herniation. A knowledgeable nursing response can be life-saving.
Understanding Intracranial Pressure (ICP)
Normal ICP ranges from 5–15 mmHg.
Sustained ICP above 20–22 mmHg requires intervention.
ICP reflects the pressure exerted by:
- Brain tissue
- Cerebrospinal fluid (CSF)
- Cerebral blood volume
According to the Monro-Kellie doctrine, the skull is a fixed space. If one component increases, another must decrease—or pressure rises.
For the RN nurse, recognizing this balance is fundamental in Neuro ICU monitoring.
Indications for ICP Monitoring
ICP monitoring is commonly used in patients with:
- Traumatic brain injury (TBI)
- Subarachnoid hemorrhage
- Intracerebral hemorrhage
- Hydrocephalus
- Severe stroke
On the NCLEX, traumatic brain injury with declining LOC is a major cue for increased ICP.
Types of ICP Monitoring Devices
1️⃣ Intraventricular Catheter (Ventriculostomy)
- Gold standard
- Measures ICP
- Allows CSF drainage
2️⃣ Subarachnoid Bolt
- Measures ICP only
- No drainage capability
3️⃣ Intraparenchymal Monitor
- Fiberoptic sensor in brain tissue
- Lower infection risk
The registered nurse must maintain strict sterile technique and level the transducer correctly to ensure accurate readings.
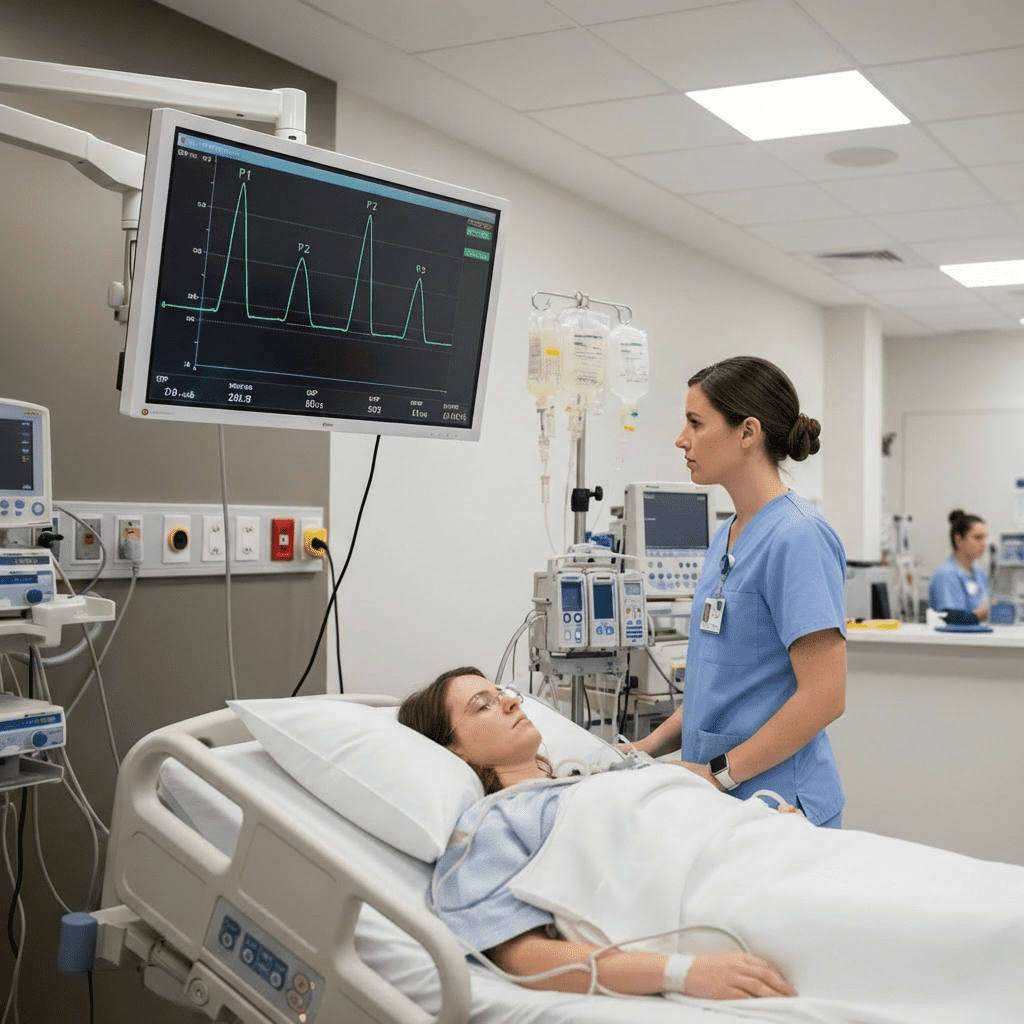
ICP Waveform Components
ICP waveforms resemble arterial waveforms but have three distinct peaks:
P1 – Percussion Wave
- Reflects arterial pulsation
- Normally the highest peak
P2 – Tidal Wave
- Reflects brain compliance
- Normally lower than P1
P3 – Dicrotic Wave
- Represents aortic valve closure
Abnormal ICP Waveform Patterns
When P2 Becomes Higher Than P1
This indicates decreased brain compliance.
This is a critical finding.
If the RN nurse observes P2 rising above P1, it signals worsening intracranial compliance and possible impending ICP elevation.
On the NCLEX, waveform changes often precede numeric ICP elevation.
When P2 becomes higher than P1, it signals decreased brain compliance and impending intracranial pressure crisis.
ICP Values and Nursing Action
| ICP Reading | Nursing Interpretation | Action |
|---|---|---|
| 5–15 mmHg | Normal | Continue monitoring |
| 16–20 mmHg | Borderline | Assess, optimize positioning |
| >20 mmHg sustained | Critical | Initiate ICP-lowering interventions |
Neuro ICU nursing bundle interventions may include:
- Elevate HOB 30 degrees
- Maintain neutral neck alignment
- Ensure adequate oxygenation
- Administer osmotic therapy (mannitol or hypertonic saline)
- Control agitation and pain
- Maintain normothermia
Cushing’s Triad: Late Sign of Increased ICP
A critical care nurse must recognize:
- Hypertension (widened pulse pressure)
- Bradycardia
- Irregular respirations
This indicates possible brainstem compression.
On the NCLEX, Cushing’s triad is a late and ominous finding.
Neuro ICU Monitoring Priorities for Nurses
ICP numbers alone do not tell the full story. The registered nurse must assess:
- Glasgow Coma Scale (GCS)
- Pupillary size and reactivity
- Motor response
- Vital signs
- CPP (Cerebral Perfusion Pressure)
CPP formula:
CPP = MAP – ICP
Goal CPP: 60–70 mmHg
Maintaining adequate CPP is the ultimate goal of neuro critical care nursing.
Leveling and Zeroing the ICP Monitor
For accurate readings, the RN nurse must:
- Level the transducer at the tragus of the ear
- Zero per institutional protocol
- Re-level after repositioning
Improper leveling can cause false ICP readings — a common NCLEX scenario.
Nursing Interventions for Elevated ICP
When ICP rises, rapid interventions are required:
- Elevate HOB to 30°
- Keep head midline
- Avoid hip flexion
- Limit suctioning
- Prevent coughing/straining
- Administer sedation as ordered
- Prepare for osmotic therapy
Cluster care should be avoided. Excess stimulation increases ICP.
This structured approach functions as a Neuro ICU nursing bundle to prevent secondary brain injury.
Sedation and ICP
Agitation increases metabolic demand and cerebral blood flow.
The RN nurse must:
- Monitor sedation level
- Prevent over-sedation
- Assess neurologic status during sedation pauses when appropriate
On the NCLEX, agitation in TBI patients requires prompt nursing action.
Complications of ICP Monitoring
The registered nurse must monitor for:
- Infection
- CSF leak
- Hemorrhage
- Catheter obstruction
Strict aseptic technique reduces infection risk.
NCLEX High-Yield ICP Review
- Normal ICP: 5–15 mmHg
- Sustained ICP >20 mmHg requires intervention
- P2 higher than P1 = decreased compliance
- Cushing’s triad = late sign
- CPP = MAP – ICP
If ICP rises suddenly, assess patient positioning first before notifying the provider.
Prioritization and assessment are key NCLEX themes.
Integrating ICP Monitoring Into Nursing Practice
Neuro ICU care requires precision, vigilance, and strong clinical judgment. The expert RN nurse must combine waveform interpretation, physical assessment, and hemodynamic monitoring to prevent secondary brain injury.
Following a structured nursing bundle approach improves:
- Patient outcomes
- Neurological preservation
- Interdisciplinary communication
- Safety in critical care settings
Final Thoughts
Intracranial pressure waveforms provide early warning signs of neurological decline. For every nurse, especially those preparing for the NCLEX or working as a registered nurse in critical care, understanding waveform interpretation is essential.
Recognizing changes such as rising ICP values or P2 elevation before clinical deterioration allows timely intervention and improved survival.
In Neuro ICU nursing, vigilance saves brain tissue — and ultimately, lives.