Heart blocks can sound scary and complicated, but they don’t have to be. For nurses, understanding them is important — because spotting a heart block early can prevent serious problems.
Let’s break down heart blocks step-by-step, using simple terms and visual tricks to help you remember them.
❤️ What is a Heart Block?
In a normal heart, electrical signals travel from the top (atria) to the bottom (ventricles) to make the heart beat in a coordinated way.
A heart block, also called an AV block (atrioventricular block), happens when these signals are delayed or completely blocked at the AV node.
👉 Key point:
- First-degree = delayed signal, but none are lost.
- Second-degree = some signals are blocked.
- Third-degree = all signals are blocked; top and bottom beat on their own, not together.
🔑 Why Do Heart Blocks Happen?
Heart blocks can happen due to:
- Aging (fibrosis of conduction system)
- Heart disease or MI (especially inferior MI)
- Medications like beta-blockers, digoxin, or calcium channel blockers
- Electrolyte imbalances (especially high potassium)
- After cardiac surgery
🔍 First-Degree AV Block
What it is:
- The electrical signal is slowed down more than normal through the AV node, but every signal still gets to the ventricles.
- It’s usually benign and does not cause symptoms.
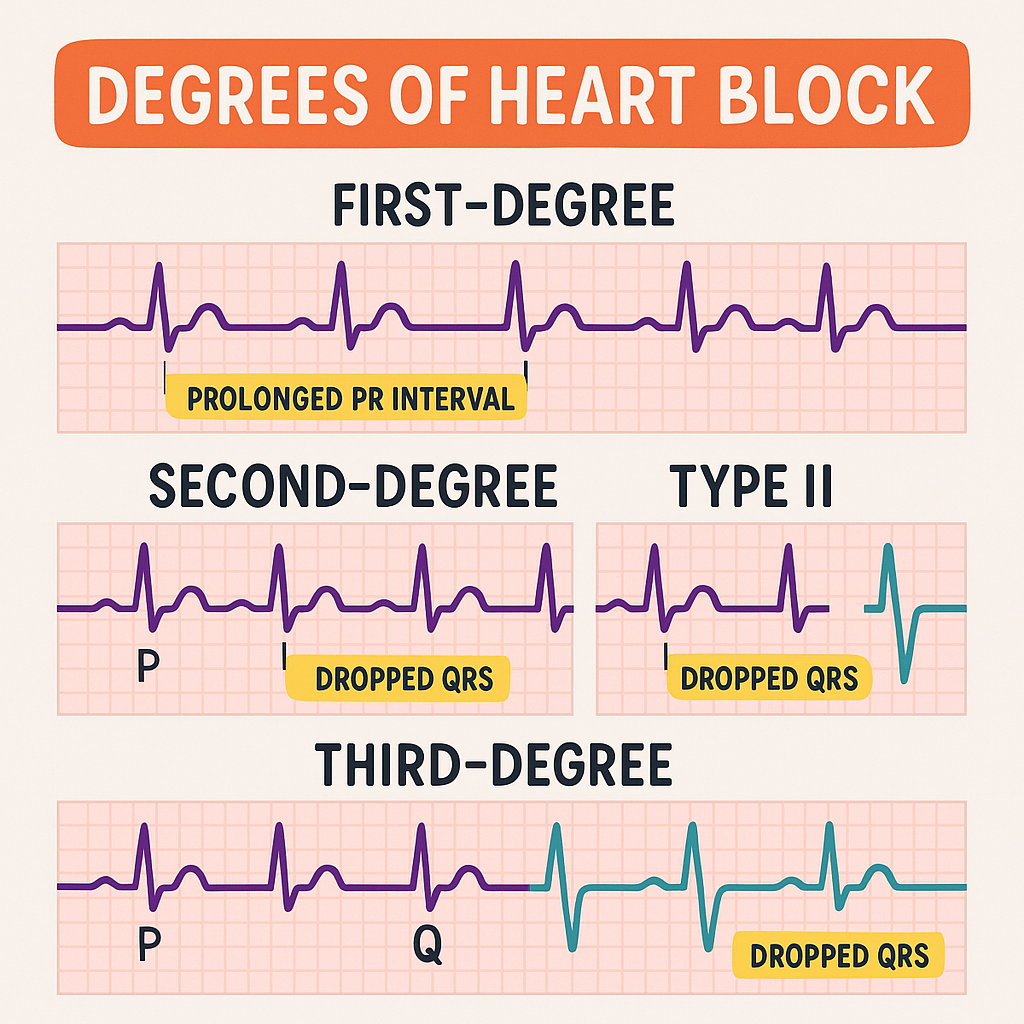
How it looks on EKG:
- PR interval is longer than 0.20 seconds (one big box).
- Every P wave still has a QRS.
How to remember:
📏 PR = Prolonged but Present
Nursing actions:
- No treatment needed in healthy patients.
- Watch for worsening block if patient is on AV-blocking meds.
- Document and monitor.
🔍 Second-Degree AV Block
Here, some signals don’t get through. There are two types: Mobitz I (Wenckebach) and Mobitz II.
Second-Degree Type I (Mobitz I or Wenckebach)
What it is:
- The PR interval gets longer and longer until one beat is dropped (QRS is missing).
- After the drop, it repeats.
How it looks on EKG:
- PR gets progressively longer → then a QRS is missing.
How to remember:
Longer, longer, longer, drop — now you have a Wenckebach!
Nursing actions:
- Usually benign, often from vagal tone or medications.
- Monitor for worsening block.
- If symptomatic bradycardia → may need atropine.
Second-Degree Type II (Mobitz II)
What it is:
- The PR interval stays the same for each conducted beat, but then suddenly, a QRS drops without warning.
- More dangerous than Type I — it can progress to complete block.
How it looks on EKG:
- PR is constant, but some P waves have no QRS.
How to remember:
If some P’s don’t get through, then you have a Mobitz II!
Nursing actions:
- This is serious. Notify the provider immediately.
- Prepare for possible pacing — this block often needs a pacemaker.
- Monitor for signs of decreased cardiac output (low BP, dizziness, syncope).
🔍 Third-Degree AV Block (Complete Heart Block)
What it is:
- The electrical signal from the atria never reaches the ventricles.
- The atria and ventricles beat independently — no coordination.
- Can cause severe bradycardia and poor cardiac output.
How it looks on EKG:
- P waves and QRS complexes have no relationship.
- Ventricular rate is very slow (20–40 bpm).
- QRS may be wide if escape rhythm is from ventricles.
How to remember:
If P’s and Q’s don’t agree, then you have a Third Degree!
Nursing actions:
- EMERGENCY. Call the provider or code team.
- Patient may need atropine (sometimes doesn’t work).
- Prepare for transcutaneous pacing until a permanent pacemaker is placed.
- Monitor airway and BP closely.
✅ Heart Block Cheat Sheet
| Type | PR Interval | QRS Dropped? | P & QRS Relationship | Risk Level |
|---|---|---|---|---|
| 1st Degree | > 0.20 sec, fixed | No | Normal | Benign |
| 2nd Degree Type I (Wenckebach) | Progressive lengthening | Yes | Pattern repeats | Usually mild |
| 2nd Degree Type II (Mobitz II) | Fixed | Yes | Random drops | Dangerous |
| 3rd Degree (Complete) | Varies | Yes | No relationship | EMERGENCY |
🗝️ Key Nursing Tips
✔️ Always check your patient — an EKG can’t tell you symptoms.
✔️ Know meds that slow AV conduction (beta-blockers, digoxin).
✔️ Monitor for hypotension, dizziness, or syncope.
✔️ Be ready for pacing if block worsens.
✔️ Communicate clearly with the provider about any change.
❤️ Heart Blocks in Real Life
Many patients live fine with a first-degree block and never notice it. But second- and third-degree blocks can cause dangerous bradycardia, syncope, and cardiac arrest.
Your job as a nurse:
- Recognize the pattern on the monitor.
- Check the patient immediately.
- Know when to call for help.
- Know the treatment: watch, med adjustment, or pacing.
📌 Key Takeaways
✅ First-Degree: Delay only. No missed beats. Usually fine.
✅ Second-Degree Type I (Wenckebach): Longer, longer, drop. Monitor.
✅ Second-Degree Type II (Mobitz II): Random drops. Dangerous. Needs pacing.
✅ Third-Degree: Total block. Emergency. Needs pacing now.
When you can quickly spot these on a strip and know what to do, you keep your patient safe and your team prepared.