Gastrointestinal (GI) bleeding is a critical topic every nurse should master, whether preparing for the NCLEX, working as a registered nurse (RN nurse), or strengthening your nursing bundle for safe patient care. Knowing how to quickly spot and respond to upper vs. lower GI bleeds is essential to save lives and prevent complications.
This simplified guide breaks down the causes, signs, and nursing interventions so you can feel confident when faced with GI bleeding scenarios.
🩸 What Is a GI Bleed?
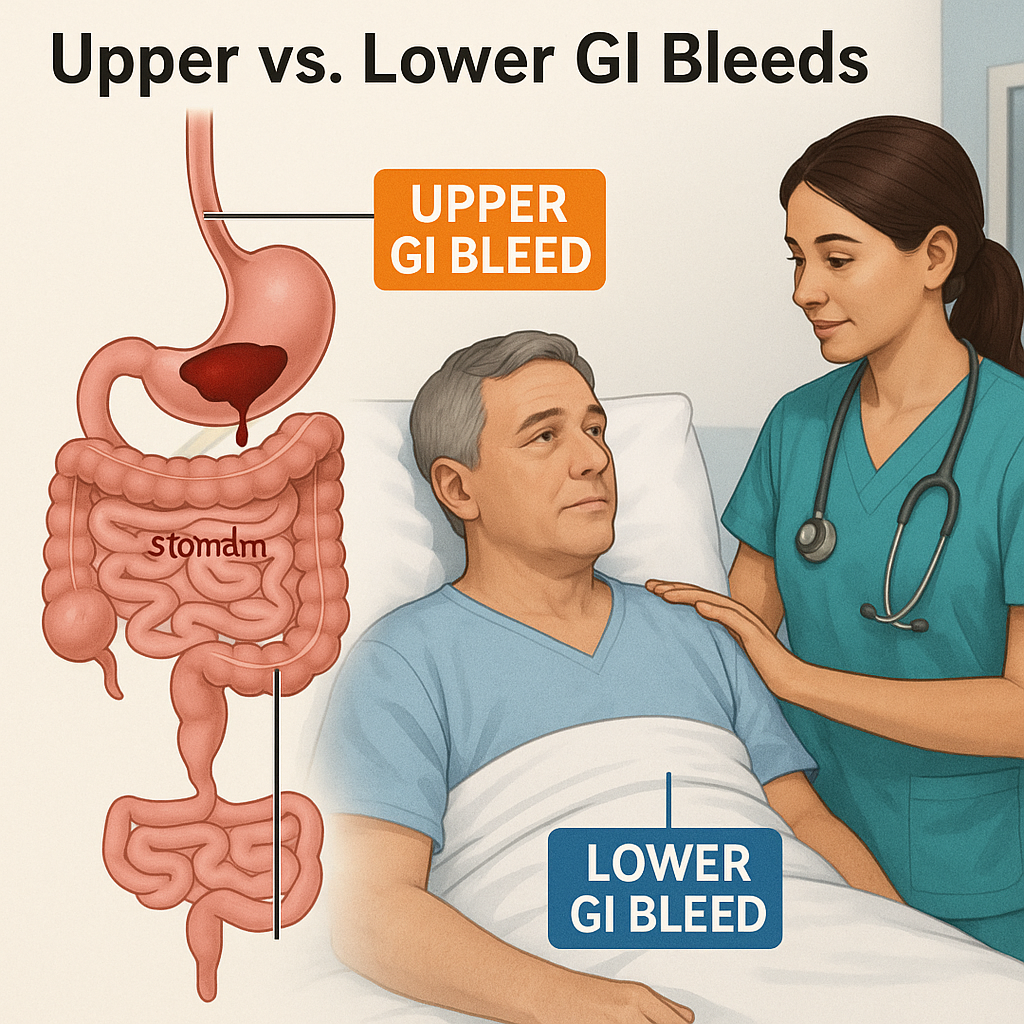
GI bleeding means there is blood loss anywhere along the digestive tract, from the esophagus to the rectum. Bleeds are generally classified as:
✅ Upper GI bleed: source is above the ligament of Treitz (esophagus, stomach, duodenum)
✅ Lower GI bleed: source is below the ligament of Treitz (small intestine, colon, rectum)
🩺 Upper GI Bleeds
Causes of Upper GI Bleeds:
- Peptic ulcer disease
- Esophageal varices
- Gastritis
- Mallory-Weiss tear
- Gastric cancer
Signs & Symptoms:
✅ Hematemesis (vomiting bright red blood or coffee-ground emesis)
✅ Melena (black, tarry stools)
✅ Weakness, dizziness, hypotension
Key Nursing Priorities for Upper GI Bleeds:
- Assess airway — patients may aspirate blood
- Place an NG tube for possible lavage
- Monitor vital signs and for hypovolemic shock
- Prepare for endoscopy
- Administer proton pump inhibitors as ordered
- Support blood transfusion needs
🩺 Lower GI Bleeds
Causes of Lower GI Bleeds:
- Diverticulosis
- Hemorrhoids
- Colorectal cancer
- Inflammatory bowel disease
- Polyps
Signs & Symptoms:
✅ Hematochezia (bright red blood per rectum)
✅ Occult blood in stool
✅ Weakness, fatigue, anemia
Key Nursing Priorities for Lower GI Bleeds:
- Monitor for hypovolemia and anemia
- Document color and amount of blood
- Administer IV fluids as needed
- Prepare for colonoscopy
- Educate patients on bowel rest and possible diet changes
- Coordinate follow-up for iron-deficiency anemia
🎯 NCLEX & Nursing Bundle Quick Facts
👉 Upper GI bleed = vomit blood, melena
👉 Lower GI bleed = bright red blood per rectum
👉 Prioritize airway, breathing, circulation (ABCs)
👉 Always check vital signs and monitor for shock
👉 Track hemoglobin/hematocrit and fluid balance
👉 Add this chart to your nursing bundle for quick reference on the floor or during NCLEX prep.
👩⚕️ Registered Nurse Priority Actions
As an RN nurse, always remember:
✅ Ensure adequate IV access (large-bore)
✅ Keep the patient on NPO until bleeding source is identified
✅ Frequent vital signs and mental status checks
✅ Coordinate labs for type & crossmatch
✅ Prepare for possible blood product administration
✅ Offer emotional support to reduce patient anxiety
🧠 Quick Memory Tips
💡 “Upper GI goes up” → vomiting blood
💡 “Lower GI goes down” → blood per rectum
💡 Coffee-ground = older upper GI bleed
💡 Hematochezia = fresh lower GI bleed
Perfect for your NCLEX studying and nursing practice!
📌 Patient Education
Upper GI Bleed Education:
- Avoid NSAIDs
- Reduce alcohol intake
- Manage H. pylori if present
Lower GI Bleed Education:
- Eat a fiber-rich diet
- Stay hydrated
- Keep up with colon cancer screenings
📚 Add to Your Nursing Bundle
✅ Upper vs. Lower GI bleed symptom chart
✅ Medication cheat sheet (PPIs, iron supplements, blood products)
✅ NCLEX-style practice questions
✅ Quick airway and shock response guide
These tools will help you as a nurse provide fast, effective, and evidence-based care.