Fluid replacement therapy is a vital aspect of patient care in all nursing settings. For every registered nurse (RN nurse), understanding how to restore and maintain a patient’s fluid balance is essential for clinical practice and NCLEX success. Whether it’s managing dehydration, shock, or electrolyte imbalance, nurses play a key role in assessing needs and administering fluids safely.
💧 What Is Fluid Replacement Therapy?
Fluid replacement therapy involves restoring body fluids lost due to illness, surgery, burns, trauma, or dehydration. The goal is to maintain proper fluid and electrolyte balance, ensuring adequate tissue perfusion and cellular function.
For nurses and nursing students, mastering this topic is critical for both NCLEX preparation and real-world patient care.
🧠 The Importance of Fluid Balance in Nursing
Water accounts for about 60% of the human body. Any disruption in this balance can lead to serious complications. Registered nurses must understand how to recognize signs of fluid volume deficit (dehydration) and fluid volume overload (excess).
Key Nursing Assessments:
- Monitor vital signs, especially blood pressure and heart rate
- Assess urine output and specific gravity
- Evaluate skin turgor and mucous membranes
- Check for edema, crackles in lungs, or weight gain
Nurses must document all findings accurately—skills emphasized in every nursing bundle designed to build strong clinical judgment.
⚗️ Types of Fluid Replacement Solutions
Fluid replacement therapy is categorized based on the type of solution used:
1. Isotonic Solutions
- Examples: 0.9% Normal Saline, Lactated Ringer’s
- Purpose: Replace extracellular fluid losses (e.g., dehydration, blood loss)
- Nursing Tip: Monitor for fluid overload in patients with heart failure or renal disease
2. Hypotonic Solutions
- Examples: 0.45% Normal Saline (½ NS)
- Purpose: Treat cellular dehydration (e.g., hypernatremia, diabetic ketoacidosis)
- Nursing Tip: Administer carefully; may cause cerebral edema if infused too rapidly
3. Hypertonic Solutions
- Examples: 3% Saline, Dextrose 10% in Water (D10W)
- Purpose: Treat hyponatremia or cerebral edema
- Nursing Tip: Monitor for signs of intravascular overload; use a central line when indicated
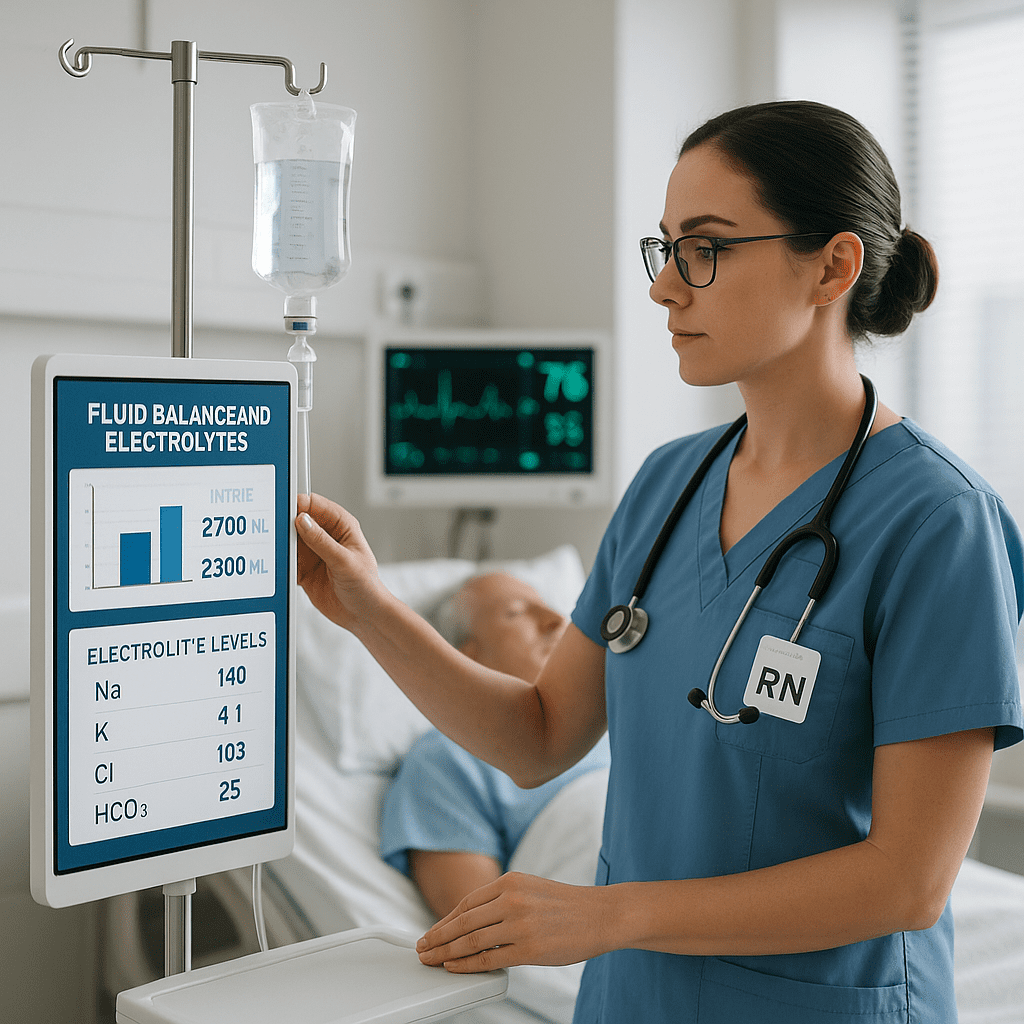
💉 Nursing Responsibilities in Fluid Therapy
Registered nurses are responsible for ensuring safe administration and monitoring throughout fluid replacement therapy.
Essential Nursing Interventions:
- Verify physician orders for type, rate, and volume of fluid.
- Use aseptic technique when inserting or maintaining IV lines.
- Monitor intake and output (I&O) hourly for critical patients.
- Observe for complications such as infiltration, phlebitis, or fluid overload.
- Document fluid administration accurately in the patient’s record.
These responsibilities align with NCLEX testing standards, focusing on patient safety and critical thinking.
⚠️ Recognizing Fluid Imbalance Complications
Fluid Volume Deficit (FVD):
- Causes: Vomiting, diarrhea, burns, hemorrhage
- Signs: Tachycardia, hypotension, dry mucous membranes, decreased urine output
- Nursing Action: Administer isotonic fluids, monitor blood pressure, assess skin turgor
Fluid Volume Overload (FVO):
- Causes: Excessive IV fluids, renal failure, heart failure
- Signs: Edema, crackles, shortness of breath, bounding pulse, increased BP
- Nursing Action: Restrict fluids, elevate head of bed, administer diuretics as prescribed
Recognizing these signs early can save lives—making it a high-priority skill for every RN nurse.
🩺 NCLEX Study Tip for Nurses
Expect NCLEX questions that test your understanding of IV fluid types and nursing priorities during fluid replacement therapy. A common test strategy is to identify which IV solution is appropriate for a specific clinical condition and what complications to monitor.
For example:
“A patient with dehydration secondary to vomiting and diarrhea is prescribed IV fluids. Which solution should the nurse expect to administer?”
✅ Correct Answer: 0.9% Normal Saline (Isotonic Solution)
📚 Why It Matters for Every Nursing Student
Understanding fluid replacement therapy helps nurses make informed decisions and prevent complications. This topic is frequently included in nursing bundles and study materials that prepare future nurses for the NCLEX and for safe clinical practice.
🧩 Key Takeaway for Registered Nurses
Fluid replacement therapy is more than just administering IV fluids—it’s about restoring homeostasis safely. Registered nurses must assess, monitor, and document every step carefully while educating patients about the importance of hydration and fluid balance. Mastering this skill ensures patient safety and professional confidence in any clinical setting.
❓Frequently Asked Questions (FAQ)
The main goal is to restore and maintain proper hydration and electrolyte balance to support organ function and circulation.
Isotonic solutions like 0.9% Normal Saline or Lactated Ringer’s are commonly used to replace fluid losses.
Nurses monitor intake and output, assess for signs of overload or deficit, and ensure proper IV administration techniques.
The NCLEX focuses on identifying appropriate fluids for conditions and recognizing complications like overload or dehydration.