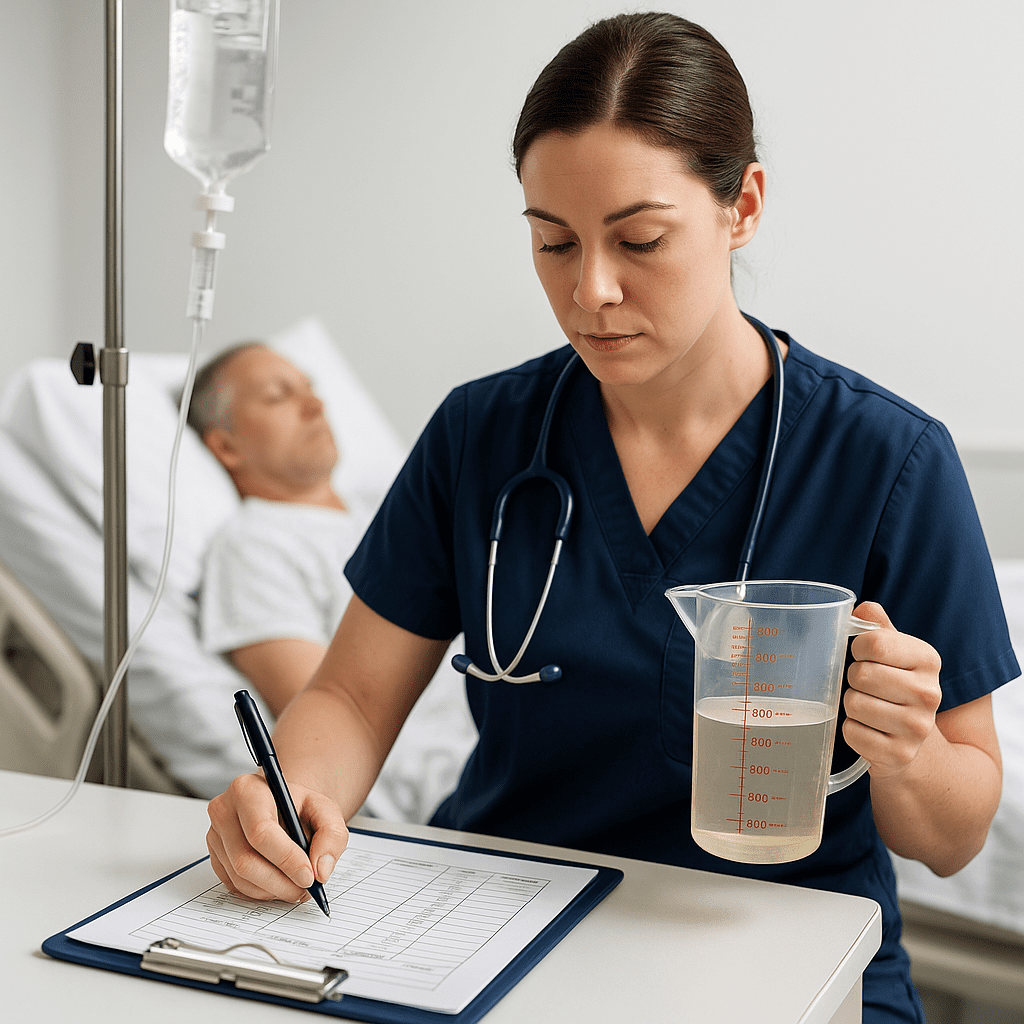
Maintaining proper fluid balance is one of the most essential parts of patient care. Every nurse, from a new graduate preparing for the NCLEX to an experienced registered nurse (RN) on the floor, must understand how to accurately monitor intake and output (I&O). This skill not only helps prevent complications but also ensures patient safety and effective treatment outcomes.
In this guide, we’ll break down fluid balance nursing into simple, easy-to-understand steps — the kind you’d find in a high-quality nursing bundle designed to make learning stress-free and effective.
💧 What Is Fluid Balance in Nursing?
Fluid balance refers to the difference between the fluids a patient takes in (intake) and the fluids that leave their body (output). Maintaining a proper balance is vital for homeostasis — keeping the body’s internal environment stable.
A positive balance means more intake than output (possible fluid overload), while a negative balance indicates more output than intake (possible dehydration or fluid deficit).
Understanding and recording this balance accurately is a key responsibility of every nurse and is often tested on the NCLEX.
🩺 Why I&O Monitoring Matters
Accurate I&O monitoring helps the RN nurse and healthcare team:
- Detect early signs of dehydration or fluid overload
- Evaluate kidney and heart function
- Guide IV therapy or medication adjustments
- Track progress in patients with chronic conditions (e.g., heart failure, renal disease)
- Support physician decision-making with precise data
In short, I&O monitoring gives valuable clues about a patient’s overall condition — something every nursing student must master before taking the NCLEX.
⚖️ What Counts as Intake and Output?
Intake
All fluids that enter the body, including:
- Oral fluids (water, juice, soups, ice chips — remember to count half the volume of melted ice chips)
- IV fluids and medications
- Tube feedings (enteral)
- Blood transfusions
Output
All fluids that leave the body, including:
- Urine (the largest portion)
- Vomit or gastric suction
- Diarrhea
- Wound drainage (e.g., from drains or dressings)
- Excess sweating (measured or estimated)
📋 Tip: Some nursing bundles include ready-to-use I&O charts and tracking templates — perfect for RN nurses who want quick and organized documentation.
🧮 How to Calculate Fluid Balance
Here’s a simple formula every nurse should memorize:
Fluid Balance = Total Intake – Total Output
- Positive balance: More intake → Possible fluid overload
- Negative balance: More output → Possible dehydration
💡 Example:
If a patient’s total intake is 2,000 mL and their total output is 1,400 mL,
→ Fluid balance = 2,000 – 1,400 = +600 mL (possible fluid retention)
On the NCLEX, expect questions that require quick calculations and interpretations just like this.
🧠 Nursing Interventions for Fluid Imbalance
If Fluid Deficit (Dehydration):
- Encourage oral fluid intake as ordered
- Administer IV fluids if prescribed
- Monitor vital signs (especially BP and HR)
- Assess for dry mucous membranes and poor skin turgor
- Evaluate urine output (color, amount, specific gravity)
If Fluid Overload:
- Restrict fluid and sodium intake
- Monitor daily weights (same time, same scale, same conditions)
- Assess for edema and lung sounds (crackles indicate fluid retention)
- Administer diuretics as ordered
- Elevate legs to reduce swelling
📝 Documentation Tips for Nurses
Accurate documentation is key to safe nursing practice and quality care. Here’s what every registered nurse should include:
- Type and amount of each fluid intake/output
- Time of recording
- Patient’s condition (edema, dry mouth, etc.)
- Any physician notifications or interventions performed
Use clear, consistent units (mL) and total the 24-hour I&O balance at the end of each shift.
🧩 Fluid Balance and the NCLEX
On the NCLEX, questions about fluid balance nursing often test:
- Recognizing signs of imbalance
- Selecting appropriate interventions
- Prioritizing actions based on assessment findings
Example question:
A patient has a urine output of 300 mL in 8 hours. What should the RN nurse do first?
✅ Answer: Assess for signs of dehydration and notify the provider.
These scenarios are core to the nursing process and appear frequently in NCLEX test plans.
💼 Practical Nursing Tips for the RN Nurse
- Always zero out your measuring container before use
- Don’t forget to record fluids in medications (like IV antibiotics)
- Educate patients on why you’re tracking their intake and output
- Collaborate with CNAs or patient care techs to ensure accuracy
- Double-check totals at the end of each shift
Small errors in I&O documentation can lead to big clinical consequences — which is why RN nurses must stay detail-oriented.
💡 Final Thoughts
Fluid balance nursing is more than just recording numbers — it’s about understanding what those numbers mean for patient health. Whether you’re preparing for the NCLEX, reviewing your nursing bundle, or practicing as a registered nurse, mastering I&O monitoring will make you a safer, more confident caregiver.
Stay consistent, stay accurate, and always think critically — because fluid balance tells a story that every nurse must learn to read.
🧾 FAQ
The normal urine output is about 30 mL/hour or 0.5–1 mL/kg/hr. Anything less may indicate dehydration or kidney dysfunction.
Typically every 8 hours, but in critical care settings, it may be done hourly.
The patient may have fluid overload, which can lead to edema or pulmonary congestion — conditions requiring prompt nursing intervention.
Yes! It’s a frequent topic in the NCLEX test plan under “Basic Care and Comfort” and “Physiological Adaptation.”
Many nursing bundles include visual charts, fluid balance worksheets, and simplified diagrams that help nursing students and RN nurses master this concept quickly.