Understanding heart blocks is a high-yield topic for the NCLEX and a must for every nurse, registered nurse (RN nurse), or nursing student. Whether you’re reviewing with a nursing bundle or preparing for clinical practice, recognizing the differences between first-degree, second-degree, and third-degree heart blocks can save lives.
🔹 What Are Heart Blocks?
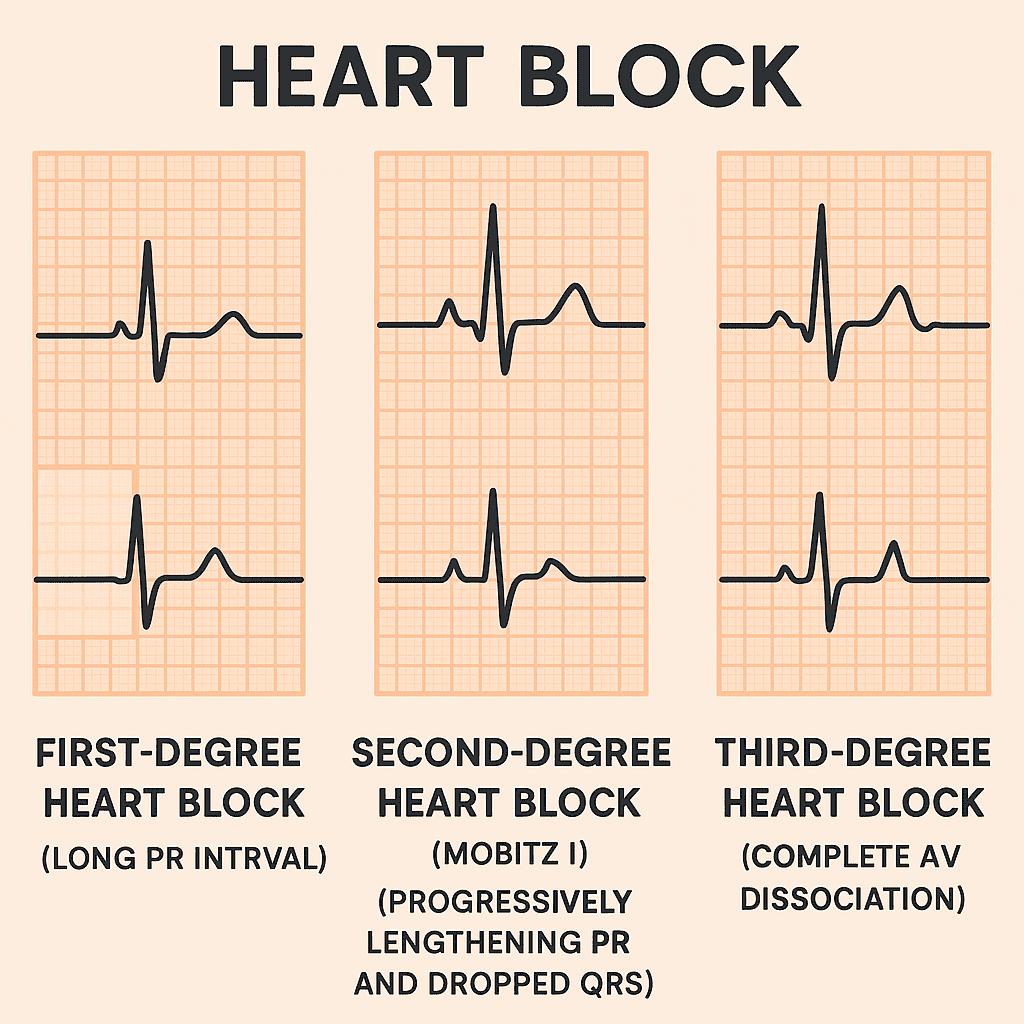
Heart blocks are conduction abnormalities where the electrical signals between the atria and ventricles are delayed or blocked. Nurses need to know how to recognize these on an ECG and understand the nursing priorities for safe patient care.
1️⃣ First-Degree Heart Block
- Definition: A consistent delay in conduction from the atria to the ventricles.
- ECG Finding: Prolonged PR interval (>0.20 seconds) but consistent.
- Symptoms: Often asymptomatic.
- Nursing Notes:
- Usually benign and may not require treatment.
- Monitor patients for progression to higher-degree blocks.
- Seen in athletes, medication effects (beta-blockers, digoxin), or electrolyte imbalances.
2️⃣ Second-Degree Heart Block
There are two main types:
➤ Mobitz Type I (Wenckebach)
- ECG Finding: PR interval progressively lengthens until a beat is dropped.
- Symptoms: May be asymptomatic or have mild dizziness.
- Nursing Notes:
- Monitor closely.
- May not require treatment unless symptomatic.
➤ Mobitz Type II
- ECG Finding: PR interval is constant, but random QRS complexes are dropped.
- Symptoms: Dizziness, syncope, or hypotension.
- Nursing Notes:
- More dangerous than Type I.
- May progress to complete (third-degree) block.
- Prepare for a pacemaker.
3️⃣ Third-Degree (Complete) Heart Block
- Definition: Complete disconnection between atrial and ventricular activity.
- ECG Finding: P waves and QRS complexes are present but not coordinated.
- Symptoms: Severe bradycardia, dizziness, syncope, risk of cardiac arrest.
- Nursing Notes:
- Medical emergency 🚨.
- Requires immediate pacing (temporary or permanent pacemaker).
- Monitor oxygen, vital signs, and prepare crash cart.
🩺 Nursing Priorities for Heart Blocks
For every nurse and RN nurse preparing for the NCLEX or working in clinical practice:
- Assess patient symptoms: dizziness, syncope, hypotension.
- Monitor ECG trends for progression.
- Check medications: beta-blockers, calcium channel blockers, digoxin can worsen blocks.
- Prepare for interventions: atropine, pacing, or emergency management in higher-degree blocks.
- Patient teaching: report new symptoms like fainting, chest pain, or palpitations immediately.
✅ Key Takeaways for NCLEX & Nursing Practice
- First-degree: Prolonged PR, usually benign.
- Second-degree Type I: PR gets longer until a beat drops.
- Second-degree Type II: Sudden dropped beats, high risk, may need pacemaker.
- Third-degree: Complete block, life-threatening, requires immediate pacing.
For the NCLEX, remember:
- “If you drop beats, you need a pacer!”
Final Thoughts
Recognizing first-degree, second-degree, and third-degree heart blocks is essential for safe patient care. Every nurse, registered nurse, or RN nurse should master these ECG findings to respond quickly in emergencies. Including this topic in your nursing bundle study plan ensures confidence for the NCLEX and real-world clinical practice.