Introduction
Electrolytes play a critical role in keeping the body’s cells, nerves, and organs functioning properly. As a nurse, knowing how to read electrolyte labs — and what to do when they’re off — is essential to providing safe, effective care.
This quick guide will walk you through the main electrolytes tested in labs, what the normal values are, what might cause abnormal levels, and how to intervene appropriately. Whether you’re preparing for a nursing exam or working in clinical care, this is information you’ll use every day.
What Are Electrolytes?
Electrolytes are minerals that carry an electric charge. They help regulate:
- Heart rhythm
- Muscle function
- Fluid balance
- Nerve signaling
- pH levels (acid-base balance)
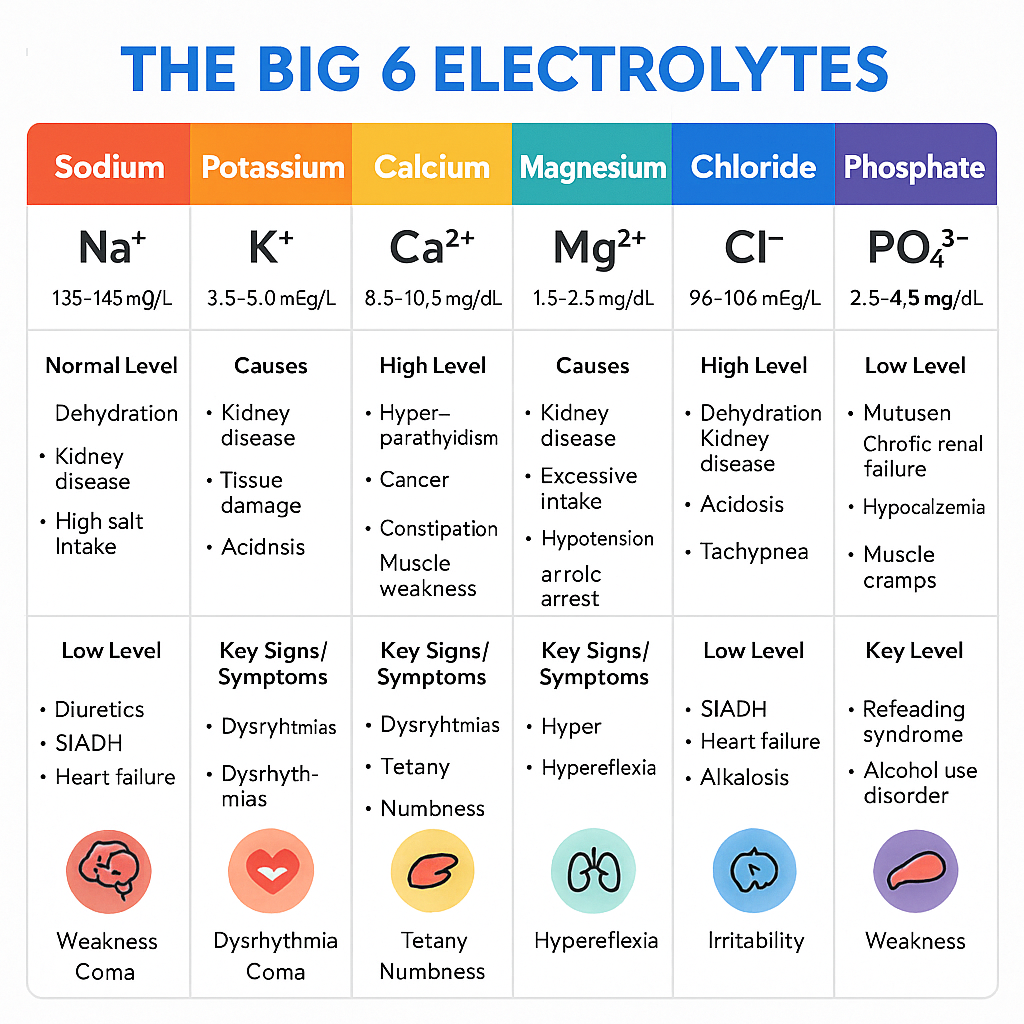
The big six electrolytes to know are:
- Sodium (Na⁺)
- Potassium (K⁺)
- Calcium (Ca²⁺)
- Magnesium (Mg²⁺)
- Chloride (Cl⁻)
- Phosphate (PO₄³⁻)
Sodium (Na⁺)
Normal Range:
135–145 mEq/L
Low Sodium: Hyponatremia
- Causes: Diuretics, vomiting, diarrhea, SIADH, heart failure
- Signs: Confusion, headache, seizures, fatigue, muscle weakness
- What to Do:
- Fluid restriction (especially in SIADH)
- Hypertonic saline (for severe symptoms)
- Monitor neuro status
- Check urine sodium and osmolality
High Sodium: Hypernatremia
- Causes: Dehydration, diabetes insipidus, excessive salt intake
- Signs: Thirst, restlessness, irritability, dry mucous membranes
- What to Do:
- Give hypotonic fluids (D5W or 0.45% NS) slowly
- Monitor I&O
- Seizure precautions if severe
Potassium (K⁺)
Normal Range:
3.5–5.0 mEq/L
Low Potassium: Hypokalemia
- Causes: Vomiting, diuretics, insulin, laxative abuse
- Signs: Muscle cramps, weakness, flat T waves on EKG, constipation
- What to Do:
- Give potassium (oral or IV; never IV push!)
- Monitor cardiac rhythm
- Recheck labs after replacement
High Potassium: Hyperkalemia
- Causes: Kidney failure, potassium-sparing diuretics, acidosis, trauma
- Signs: Peaked T waves, muscle weakness, cardiac arrest risk
- What to Do:
- Administer insulin with D50
- Calcium gluconate (to protect heart)
- Kayexalate, diuretics, or dialysis
- Continuous EKG monitoring
Calcium (Ca²⁺)
Normal Range:
8.5–10.5 mg/dL
Low Calcium: Hypocalcemia
- Causes: Hypoparathyroidism, vitamin D deficiency, pancreatitis
- Signs: Muscle spasms, tingling, Chvostek’s and Trousseau’s signs
- What to Do:
- IV calcium gluconate
- Oral calcium and vitamin D
- Monitor for tetany or laryngospasm
High Calcium: Hypercalcemia
- Causes: Hyperparathyroidism, cancer, thiazide diuretics
- Signs: Lethargy, constipation, kidney stones, bone pain
- What to Do:
- IV fluids to dilute calcium
- Loop diuretics (not thiazides!)
- Bisphosphonates if due to cancer
Magnesium (Mg²⁺)
Normal Range:
1.6–2.6 mg/dL
Low Magnesium: Hypomagnesemia
- Causes: Alcohol abuse, diarrhea, malnutrition
- Signs: Muscle cramps, tremors, increased reflexes, EKG changes (torsades de pointes)
- What to Do:
- IV magnesium sulfate
- Monitor deep tendon reflexes
- Recheck levels often
High Magnesium: Hypermagnesemia
- Causes: Kidney failure, overuse of magnesium-based antacids or laxatives
- Signs: Weakness, low BP, bradycardia, decreased reflexes
- What to Do:
- Stop magnesium intake
- Calcium gluconate IV
- Dialysis if severe
Chloride (Cl⁻)
Normal Range:
97–107 mEq/L
Chloride often follows sodium and is involved in maintaining acid-base balance.
- Hypochloremia: Often occurs with vomiting, NG suctioning, or hyponatremia
- Hyperchloremia: Can be caused by dehydration or kidney issues
- What to Do: Focus on correcting the underlying sodium or fluid issue.
Phosphate (PO₄³⁻)
Normal Range:
2.5–4.5 mg/dL
Low Phosphate: Hypophosphatemia
- Causes: Alcoholism, refeeding syndrome, DKA
- Signs: Muscle weakness, respiratory failure, confusion
- What to Do:
- Oral or IV phosphate
- Monitor labs frequently
High Phosphate: Hyperphosphatemia
- Causes: Chronic kidney disease, tumor lysis syndrome
- Signs: Often asymptomatic, but can cause hypocalcemia symptoms
- What to Do:
- Phosphate binders (calcium acetate)
- Dietary phosphate restriction
How to Remember the Electrolyte Effects
Use the “Think by System” method:
| System | Affected Electrolytes | What to Watch |
|---|---|---|
| Heart | K⁺, Ca²⁺, Mg²⁺ | EKG changes, arrhythmias |
| Muscles | Ca²⁺, Mg²⁺, K⁺ | Weakness, cramping, reflexes |
| Nerves/Brain | Na⁺, Ca²⁺ | Confusion, seizures, LOC |
| Kidneys | All | Creatinine, urine output, retention or wasting |
Tips for Nurses
- Always check trends, not just single values.
- Know your facility’s electrolyte replacement protocols.
- Recheck labs after any correction.
- Watch the rate of IV replacements — especially potassium and magnesium.
- Use telemetry when correcting major shifts.
- Educate patients on food and medications that affect their electrolytes.
Sample Cheat Sheet Summary
| Electrolyte | Normal Range | Main Concern When Low | Main Concern When High |
|---|---|---|---|
| Sodium | 135–145 mEq/L | Seizures | Dehydration, neuro changes |
| Potassium | 3.5–5.0 mEq/L | Arrhythmias | Cardiac arrest |
| Calcium | 8.5–10.5 mg/dL | Tetany, spasms | Constipation, stones |
| Magnesium | 1.6–2.6 mg/dL | Tremors, seizures | Bradycardia, weakness |
| Chloride | 97–107 mEq/L | Vomiting, alkalosis | Acidosis |
| Phosphate | 2.5–4.5 mg/dL | Weakness, confusion | Hypocalcemia symptoms |
Conclusion
Electrolyte labs are more than just numbers — they tell the story of what’s happening inside your patient. Knowing what’s normal, what’s not, and how to respond makes you a safer, more effective nurse.
Keep this guide nearby during clinicals, exams, or when you’re reviewing labs on your shift. With time, recognizing and correcting electrolyte imbalances will become second nature.