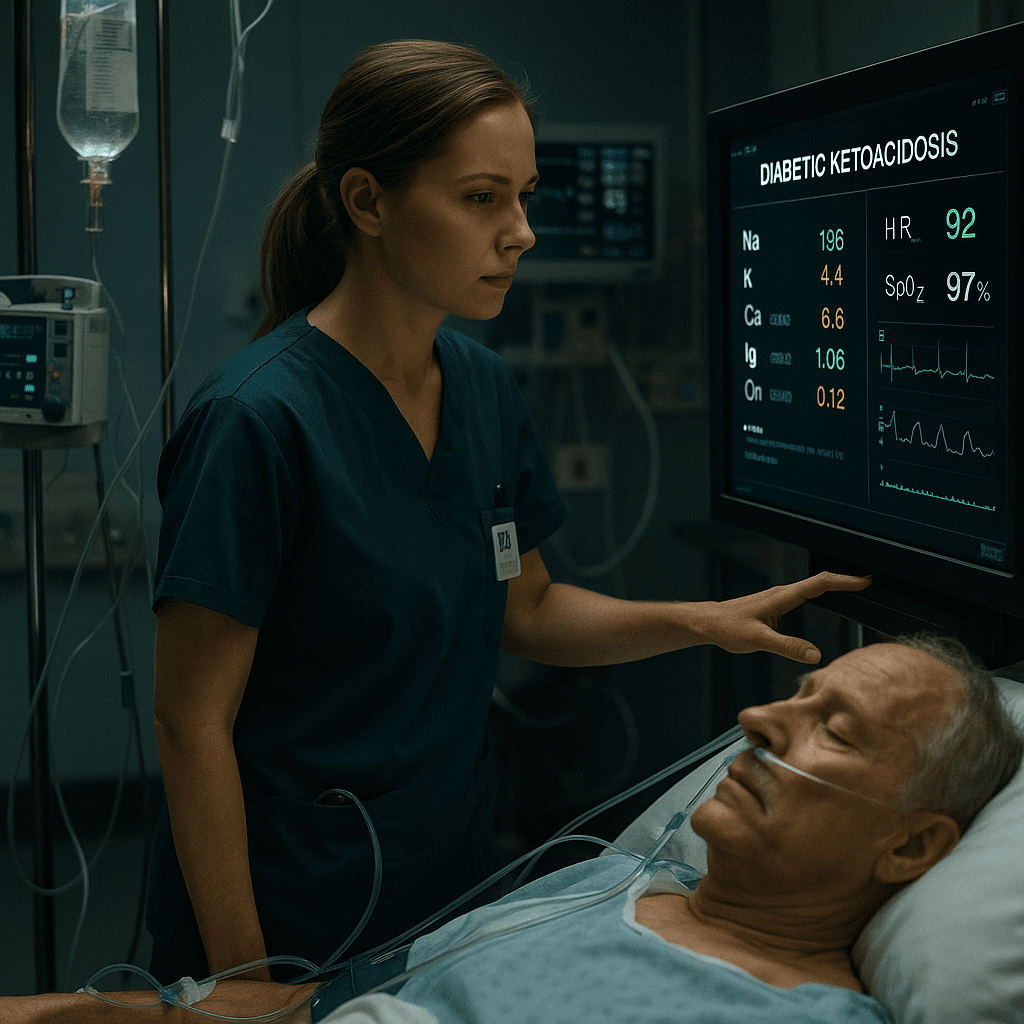
Diabetic Ketoacidosis (DKA) is a life-threatening emergency every registered nurse (RN nurse) must be ready to manage. It occurs when the body cannot use glucose due to insulin deficiency, leading to fat breakdown and ketone accumulation.
But the hidden danger in DKA isn’t only high blood sugar — it’s electrolyte imbalance, which can cause cardiac dysrhythmias, shock, and even death if untreated.
Understanding electrolyte shifts in DKA is a vital NCLEX topic and a cornerstone for safe nursing practice in emergency and critical care.
Key Electrolytes Affected in DKA
When insulin is absent, the body burns fat for energy, leading to acidic ketones in the blood. This triggers osmotic diuresis, which flushes water and electrolytes from the body — mainly potassium (K⁺), sodium (Na⁺), and phosphate (PO₄³⁻).
Let’s break down the most important ones every nurse should understand.
🧪 1. Potassium (K⁺): The Most Critical Electrolyte
Normal range: 3.5–5.0 mEq/L
What Happens in DKA:
- Potassium leaves cells due to acidosis.
- Serum potassium may appear normal or high initially.
- As insulin therapy begins, potassium shifts back into cells, leading to dangerous hypokalemia.
Clinical Signs:
- Muscle weakness
- Cardiac dysrhythmias
- Shallow respirations
Nursing Interventions:
- Monitor cardiac rhythm continuously.
- Check potassium before giving insulin.
- Administer potassium supplements when levels start to fall.
- For the NCLEX, remember: Never start insulin in DKA until potassium is above 3.3 mEq/L.
💧 2. Sodium (Na⁺): The Water Balance Marker
Normal range: 135–145 mEq/L
What Happens in DKA:
- Excess glucose causes osmotic diuresis, leading to sodium loss in urine.
- Severe dehydration lowers sodium, but corrected sodium may appear high due to hyperglycemia.
Nursing Interventions:
- Monitor serum sodium and hydration status.
- Calculate corrected sodium using this NCLEX-favorite formula:
Corrected Na⁺ = Measured Na⁺ + (1.6 × [(Glucose – 100) ÷ 100]) - Administer IV fluids (usually isotonic saline) to restore balance gradually.
⚡ 3. Phosphate (PO₄³⁻): The Hidden Danger
Normal range: 2.5–4.5 mg/dL
What Happens in DKA:
- Phosphate is lost in urine due to osmotic diuresis.
- Low phosphate leads to muscle weakness and respiratory failure.
Nursing Interventions:
- Monitor phosphate levels closely during insulin therapy.
- Replace phosphate if levels drop below 1.0 mg/dL or if muscle weakness develops.
- For NCLEX, associate phosphate deficiency with weak respiratory muscles and potential ventilatory failure.
🔥 4. Magnesium (Mg²⁺) and Calcium (Ca²⁺): The Supporting Electrolytes
Although less emphasized, magnesium and calcium can fluctuate during DKA correction.
- Low magnesium may worsen cardiac instability.
- Calcium may decrease as phosphate levels rise during treatment.
Nursing Tip: Always review comprehensive electrolyte panels, especially in critically ill patients receiving insulin and fluids.
Nursing Priorities in DKA Management
A registered nurse or RN nurse should always follow the DKA treatment triad:
- Fluids – to correct dehydration.
- Insulin – to reduce blood glucose and stop ketone production.
- Electrolyte replacement – to restore cellular function and prevent arrhythmias.
NCLEX Insight:
During DKA management, if the nurse gives insulin before correcting potassium, the patient can develop fatal hypokalemia. Always check potassium first!
Critical Thinking for Nursing Students
Scenario:
A patient with DKA has potassium of 3.0 mEq/L. The provider orders IV insulin.
Question:
What should the nurse do first?
✅ Hold insulin and notify the provider. Administer potassium before starting insulin.
This type of question is classic on the NCLEX and tests a nurse’s ability to prioritize care safely.
Conclusion
Electrolyte imbalances in diabetic ketoacidosis can be subtle yet deadly. For every nurse and registered nurse, mastering these shifts ensures faster intervention, safer insulin therapy, and better patient outcomes.
For nursing students preparing for the NCLEX, remember:
👉 Always think “Potassium before Insulin”
👉 Always monitor sodium, phosphate, and magnesium
👉 Always reassess after each intervention
FAQ
Potassium. Always ensure levels are above 3.3 mEq/L.
Insulin drives phosphate into cells, and diuresis increases phosphate loss.
Usually 0.9% Normal Saline or 0.45% Saline once stable.
Hypokalemia, as it can lead to cardiac arrest.
Monitor potassium before insulin and watch ECG for arrhythmias.