Diabetes Mellitus remains one of the most common chronic illnesses nurses encounter in clinical practice. Because of its complexity, NCLEX questions frequently focus on glucose monitoring, insulin administration, and patient education. As an RN nurse or nursing student, mastering these concepts is essential for safe and effective care. Whether you’re preparing for exams or building skills at the bedside, this guide breaks down what every registered nurse must know.
✅ Understanding Diabetes Mellitus
Diabetes Mellitus is a metabolic disorder marked by high blood glucose levels. However, the underlying cause varies:
- Type 1 Diabetes: The pancreas produces little or no insulin.
- Type 2 Diabetes: The body becomes resistant to insulin or produces insufficient amounts.
- Gestational Diabetes: Glucose intolerance that occurs during pregnancy.
Because insulin impacts every cell, poor management can lead to complications such as DKA, HHS, neuropathy, nephropathy, and cardiovascular disease. Consequently, nurses must monitor patients closely and act quickly when glucose levels fall outside the normal range.
✅ Blood Glucose Monitoring: What Nurses Must Do
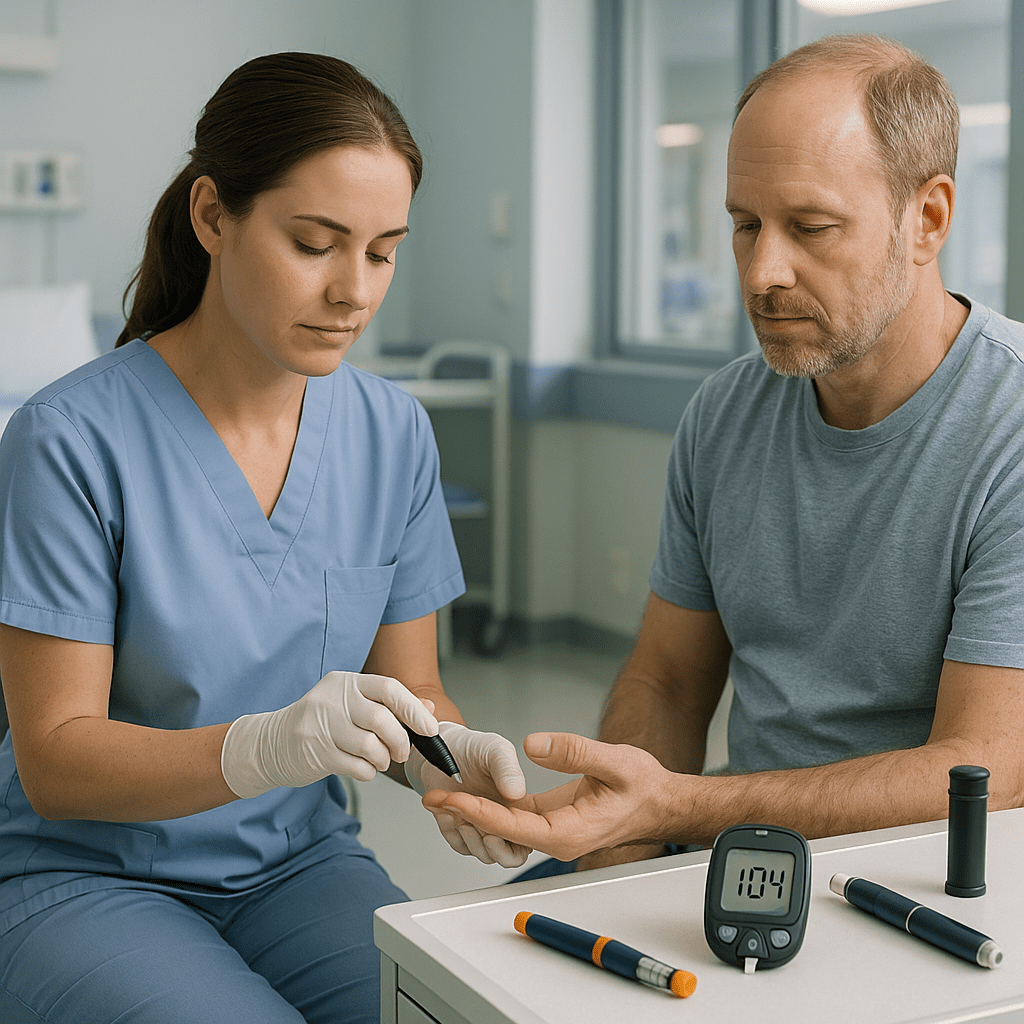
Accurate monitoring helps prevent emergencies and guides treatment.
1. Bedside Glucose Checks
Most hospitalized diabetic patients need regular glucose checks. Additionally:
- Perform checks before meals and at bedtime.
- Ensure the finger is warm and has good circulation.
- Avoid “milking” the finger excessively to prevent false readings.
2. Lab Measurements
Fasting glucose and HbA1c help evaluate long-term control. Typically:
- HbA1c < 7% indicates good control.
- Values above 9% show poor management and higher complication risk.
As an RN nurse, your role includes recognizing abnormal values and notifying providers promptly.
✅ Insulin Therapy: Types and Nursing Responsibilities
Insulin is a core topic in every nursing bundle and appears repeatedly on the NCLEX.
🔹 Types of Insulin
Insulin is categorized by onset, peak, and duration:
| Type | Example | Onset | Peak | Duration |
|---|---|---|---|---|
| Rapid-acting | Lispro, Aspart | 10–30 mins | 30–90 mins | 3–5 hrs |
| Short-acting | Regular | 30–60 mins | 2–5 hrs | 5–8 hrs |
| Intermediate | NPH | 1–2 hrs | 4–12 hrs | 14–24 hrs |
| Long-acting | Glargine, Detemir | 1–2 hrs | No peak | 24 hrs |
| Ultra–long | Degludec | 1 hr | No peak | 42 hrs |
✅ Insulin Administration: Critical Nursing Steps
Because insulin errors can be fatal, nurses must follow strict precautions.
1. Use the Correct Insulin
Always verify:
- Type
- Dose
- Timing
- Patient identity
- Double-check high-alert medications with another nurse.
2. Rotate Injection Sites
This prevents lipodystrophy and ensures proper absorption.
Common sites include:
- Abdomen
- Thighs
- Upper arms
3. Know Peak Times
Hypoglycemia most often occurs during insulin peak action. Therefore, close monitoring is essential.
4. Mixed Insulin Safety
When mixing NPH and Regular insulin:
✅ CLEAR (Regular) before CLOUDY (NPH)
❌ Never mix long-acting insulins like Glargine.
✅ Recognizing Hypoglycemia and Hyperglycemia
Hypoglycemia (blood glucose < 70 mg/dL):
- Sweating
- Tremors
- Palpitations
- Confusion
- Irritability
Immediate treatment:
Give 15 g of fast-acting glucose → recheck in 15 minutes.
Hyperglycemia:
- Polyuria
- Polydipsia
- Polyphagia
- Blurred vision
In hospital settings, uncontrolled hyperglycemia increases infection risk and prolongs healing.
✅ Nursing Priorities for Diabetic Patients
A registered nurse must prioritize:
✅ 1. Monitoring vital signs and glucose
✅ 2. Watching for insulin reactions
✅ 3. Educating patients on food choices, carb counting, and sick-day rules
✅ 4. Teaching injection techniques
✅ 5. Preventing complications like DKA and hypoglycemia
Because diabetes impacts multiple body systems, these steps appear in most NCLEX exams and clinical simulation labs.
✅ Patient Education: Your Key NCLEX Skill
Teaching improves patient safety. Nurses should educate patients on:
- Rotating injection sites
- Storing insulin properly
- Carrying fast-acting carbs
- Checking blood glucose regularly
- Recognizing early signs of hypo- and hyperglycemia
Strong education skills also help you build confidence as an RN nurse providing holistic care.
✅ Conclusion
Diabetes management is a core competency in modern nursing practice. From monitoring glucose to administering insulin safely, nurses play a crucial role in preventing complications. Understanding these principles not only improves patient outcomes but also boosts your performance on the NCLEX and in real-world clinical scenarios. For deeper learning, consider adding a nursing bundle on diabetes and endocrine disorders to your study materials.
FAQs About Diabetes Mellitus
The primary goal is to maintain blood glucose within a safe range to prevent both acute and long-term complications. A registered nurse uses glucose monitoring to guide insulin therapy, detect hyperglycemia or hypoglycemia early, and adjust patient education. This is heavily tested on the NCLEX because it reflects essential bedside nursing responsibilities.
The frequency depends on the patient’s condition and treatment plan. Critically ill patients may require monitoring every 1–2 hours, while stable patients might need checks before meals and at bedtime. RN nurses follow provider orders and facility protocols, but must recognize when additional checks are clinically necessary.
A nursing bundle for diabetes usually includes these insulin types:
Rapid-acting: Lispro, Aspart
Short-acting: Regular insulin
Intermediate-acting: NPH
Long-acting: Glargine, Detemir