👶 Why Nurses Must Know About Pediatric Dehydration
Dehydration in kids is one of the most common pediatric problems registered nurses (RNs) face—especially in ER, pediatric, and med-surg settings. Because children have smaller fluid reserves than adults, they can deteriorate quickly. Understanding how to recognize the signs, assess severity, and provide appropriate fluid replacement is a core skill for every nurse, especially for those studying for the NCLEX.
🚨 Common Causes of Dehydration in Children
Before jumping into signs and symptoms, it helps to understand why kids get dehydrated:
- Vomiting and diarrhea (often from viral illnesses)
- Fever
- Poor fluid intake
- Hot weather/overheating
- Increased fluid loss from illnesses (like diabetes or burns)
For nurses, recognizing risk factors early helps prevent complications.
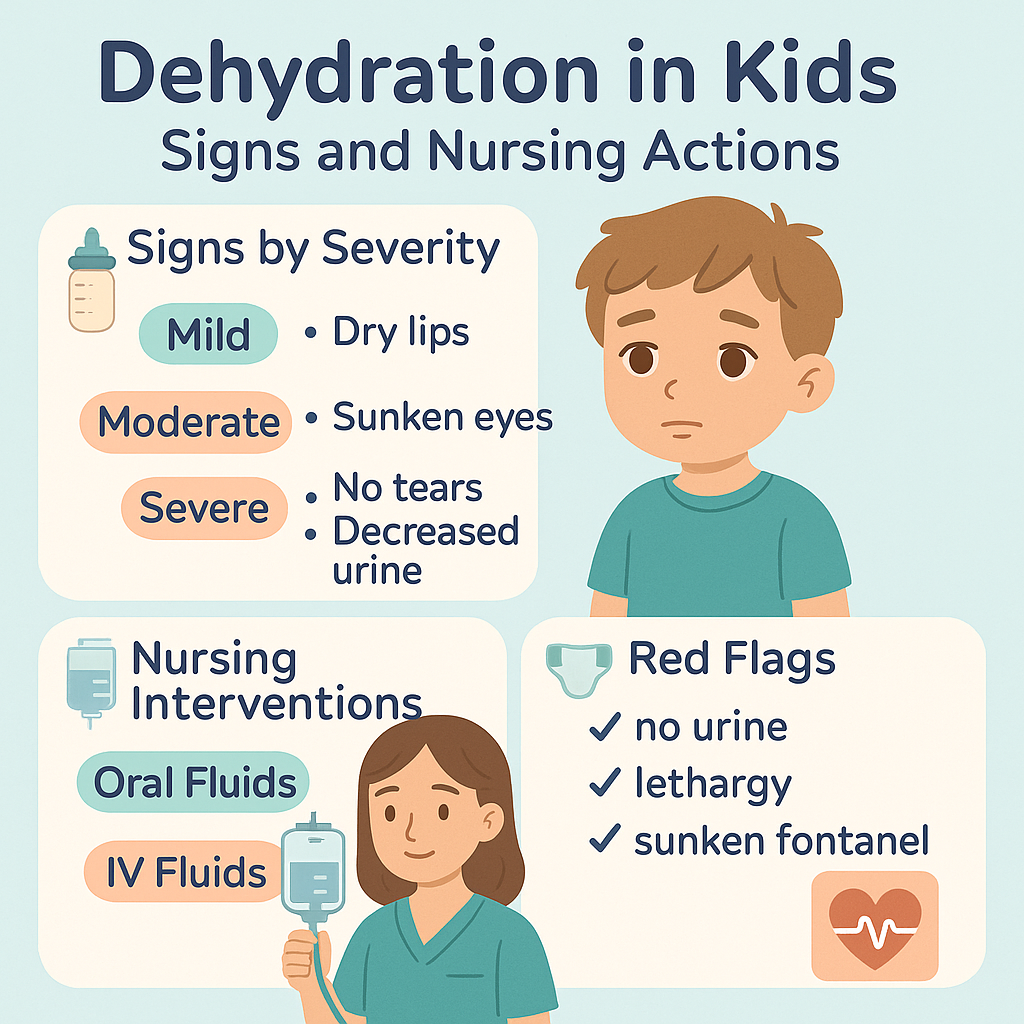
🧠 Key Nursing Assessment: Signs of Dehydration in Children
Here’s a quick nursing cheat sheet for assessing dehydration severity:
Mild Dehydration
- Slightly dry lips/mouth
- Normal activity level
- Thirsty but alert
- Urinating less than usual
Moderate Dehydration
- Dry mucous membranes
- Sunken eyes
- Irritability or lethargy
- Decreased urine output
- Increased heart rate
Severe Dehydration
- Very dry mouth
- Cool, mottled skin
- Sunken fontanel (in infants)
- No tears when crying
- Weak or absent pulses
- Hypotension
- Delayed capillary refill > 2 seconds
👉 NCLEX Tip: Capillary refill and skin turgor are key signs to check in pediatric dehydration assessments.
🧪 Lab Values to Know (NCLEX Alert!)
Dehydration may cause the following lab changes:
- ↑ Sodium (hypernatremia)
- ↑ Hematocrit
- ↑ BUN and creatinine
- ↓ Urine output with dark color and high specific gravity
Always correlate labs with physical signs for a complete nursing assessment.
💧 How to Replace Fluids: A Nursing Breakdown
1. Oral Rehydration (Mild to Moderate)
Use oral rehydration solution (ORS), like Pedialyte:
- Small, frequent sips
- 5–10 mL every 5 minutes for vomiting children
- Avoid sugary drinks and soda—they can worsen diarrhea
⏱️ RN Nurse Tip: If a child can drink and is not vomiting uncontrollably, ORS is preferred over IV fluids.
2. IV Fluid Replacement (Moderate to Severe)
Used when:
- Child can’t tolerate oral intake
- Signs of shock or severe dehydration present
Common IV Fluids:
- 0.9% NS (Normal Saline)
- D5NS with potassium (only if child has voided)
- Monitor I&O closely
📦 Include this knowledge in your nursing bundle of pediatric care flashcards!
🧍♀️ Nursing Interventions You Need to Know
Here are the top NCLEX-focused interventions for dehydration in kids:
| Intervention | Nursing Action |
|---|---|
| Monitor I&O | Weigh diapers, track oral and IV fluids |
| Daily weights | Use same time, scale, and clothing |
| Vitals signs | Watch HR, BP, temp for worsening signs |
| Educate parents | Teach fluid goals, signs of dehydration |
| Skin assessment | Look for turgor, dryness, and cap refill |
🚩 Red Flags Nurses Should Never Ignore
Every RN nurse and nursing student must respond immediately if these appear:
- No urine in 8+ hours
- Listlessness or unresponsiveness
- Rapid breathing or weak pulse
- Seizures (may result from severe electrolyte imbalances)
🏥 Call the provider and prepare for IV therapy if these are present.
🗣️ Nurse’s Role in Family Education
Nurses are not just caregivers—they’re educators. It’s vital to teach parents about:
- Proper hydration at home
- When to seek emergency care
- Safe oral rehydration options
- Preventing dehydration during illness
Use therapeutic communication and explain simply:
“Your child needs more fluids to stay strong and fight off the illness.”
✅ Quick Review Questions (NCLEX Style)
Q1: What is the earliest sign of dehydration in a 2-year-old?
A. Sunken fontanel
B. Hypotension
C. Dry lips and increased thirst
D. Bradycardia
✔️ Answer: C
Q2: A child with diarrhea is lethargic and has no tears. What is the nurse’s best first action?
A. Give apple juice
B. Administer IV fluids as ordered
C. Encourage deep breathing
D. Give a popsicle
✔️ Answer: B
🧠 Final Thoughts for Nurses and Students
Whether you’re preparing for the NCLEX, building your nursing bundle, or working as a registered nurse, knowing how to assess and manage dehydration in kids is essential. Early recognition and fast intervention can prevent complications and save lives.
This topic is a high-yield focus for pediatric care on exams and in clinical practice.