Agitation can escalate quickly in healthcare settings. Therefore, effective de-escalation remains a critical skill for every registered nurse. By using structured techniques, a nurse can reduce tension, protect safety, and maintain therapeutic relationships. These strategies appear frequently in psychiatric nursing practice and on the NCLEX, making them essential for every RN nurse.
Understanding Agitation in Clinical Settings
Agitation may arise from pain, fear, mental illness, substance use, or environmental stressors. As a result, patients may display pacing, raised voices, clenched fists, or verbal aggression. Early recognition allows the registered nurse to intervene before behaviors escalate.
Additionally, agitation often signals unmet needs. When a nurse identifies triggers, care becomes more patient-centered and effective. Many nursing bundle resources emphasize this assessment-first approach because it aligns with safety-focused nursing standards.
Core Principles of De-Escalation in Nursing
Successful de-escalation begins with self-control. First, the RN nurse maintains a calm tone and relaxed posture. Next, respectful communication builds trust and reduces perceived threats.
Moreover, personal space matters. Standing at an angle and keeping a safe distance help the patient feel less cornered. Clear boundaries, combined with empathy, allow the nurse to guide behavior without confrontation.
Verbal De-Escalation Techniques Nurses Use
Verbal strategies form the foundation of de-escalation. The registered nurse uses simple, clear language and avoids arguing. Instead of giving orders, nurses offer choices to restore patient autonomy.
For example, statements such as “I want to help you feel safer” or “Let’s find a solution together” reduce resistance. These therapeutic communication skills receive strong emphasis in nursing bundle programs and are frequently tested on the NCLEX.
Nonverbal De-Escalation Strategies
Nonverbal cues strongly influence patient behavior. Maintaining open body language, appropriate eye contact, and slow movements signals safety. Meanwhile, reducing environmental stimuli—such as noise and crowding—supports emotional regulation.
In addition, the RN nurse positions themselves near exits when needed to ensure personal safety. These actions demonstrate situational awareness, a key element of safe nursing practice.
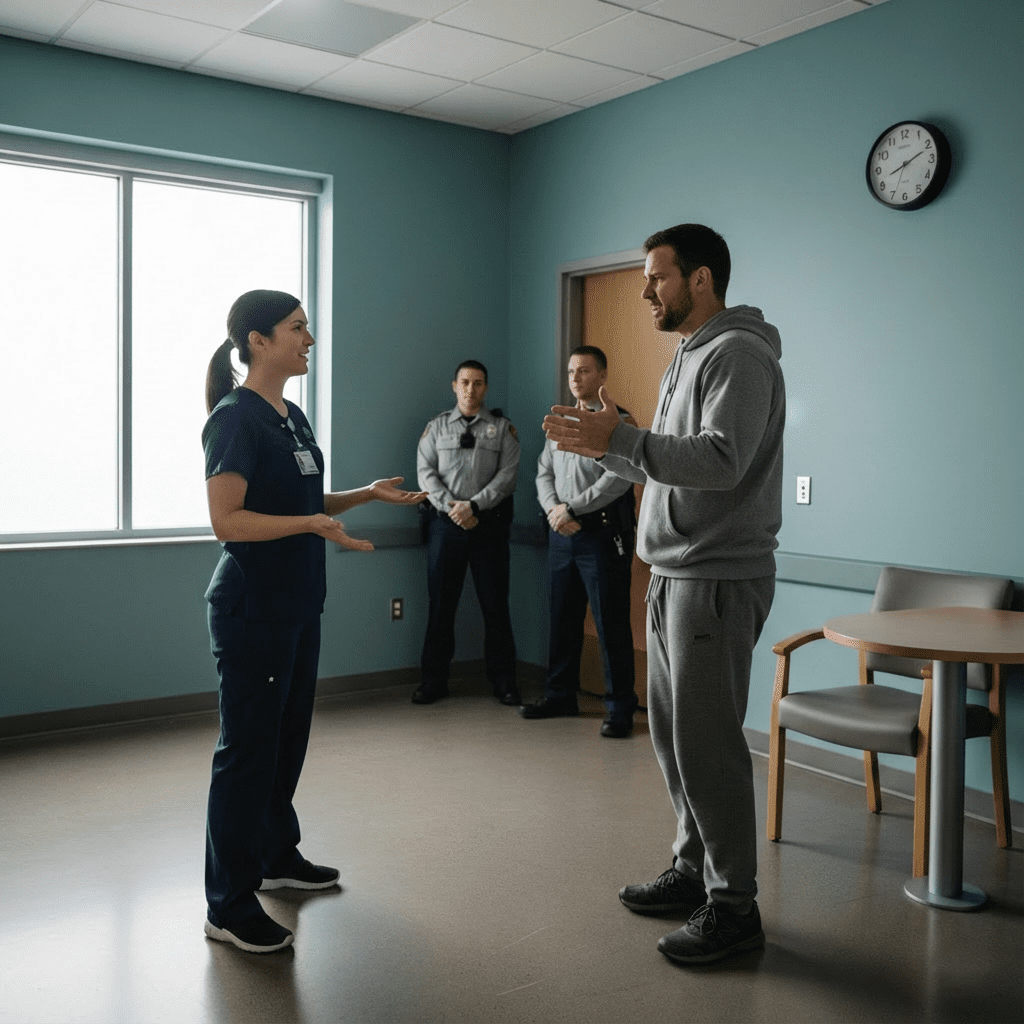
Safety and Team-Based De-Escalation
Sometimes, individual efforts are not enough. In such cases, the registered nurse activates team support early. Clear communication with colleagues prevents confusion and enhances patient safety.
If de-escalation fails, nurses follow facility protocols for medication, restraints, or seclusion as last-resort measures. Importantly, ethical and legal guidelines govern these interventions, and they remain high-priority topics on the NCLEX.
Teaching Patients Self-Regulation Skills
Education supports long-term outcomes. After a crisis, the nurse helps patients identify triggers and coping strategies. Techniques such as deep breathing, grounding exercises, and requesting help early empower patients.
By reinforcing these skills, the RN nurse promotes independence and emotional awareness. This educational role reflects holistic nursing care beyond crisis management.
NCLEX Focus: De-Escalation and Patient Safety
On the NCLEX, de-escalation questions often test priority actions, communication techniques, and safety principles. Typically, correct answers emphasize calm behavior, least-restrictive interventions, and patient dignity. Reviewing these concepts in a comprehensive nursing bundle strengthens exam readiness.
Conclusion
De-escalation techniques protect both patients and healthcare providers. Through early assessment, calm communication, and structured interventions, every registered nurse can reduce agitation safely. Whether preparing for the NCLEX or practicing at the bedside, every RN nurse benefits from mastering evidence-based nursing de-escalation strategies.
✅ FAQ
De-escalation techniques are strategies a nurse uses to calm agitated or aggressive patients through communication, body language, and environmental control. These methods help prevent violence and maintain patient safety in nursing care.
De-escalation protects patients, staff, and visitors from harm. It also reduces the need for restraints or medications. Because patient safety is a priority, these techniques are commonly tested on the NCLEX.
The registered nurse first ensures personal and patient safety, then uses calm verbal communication and maintains appropriate distance. Early intervention often prevents further escalation.
RN nurses use a calm tone, simple language, empathy, and choices. Statements that acknowledge feelings without judgment help patients regain emotional control.