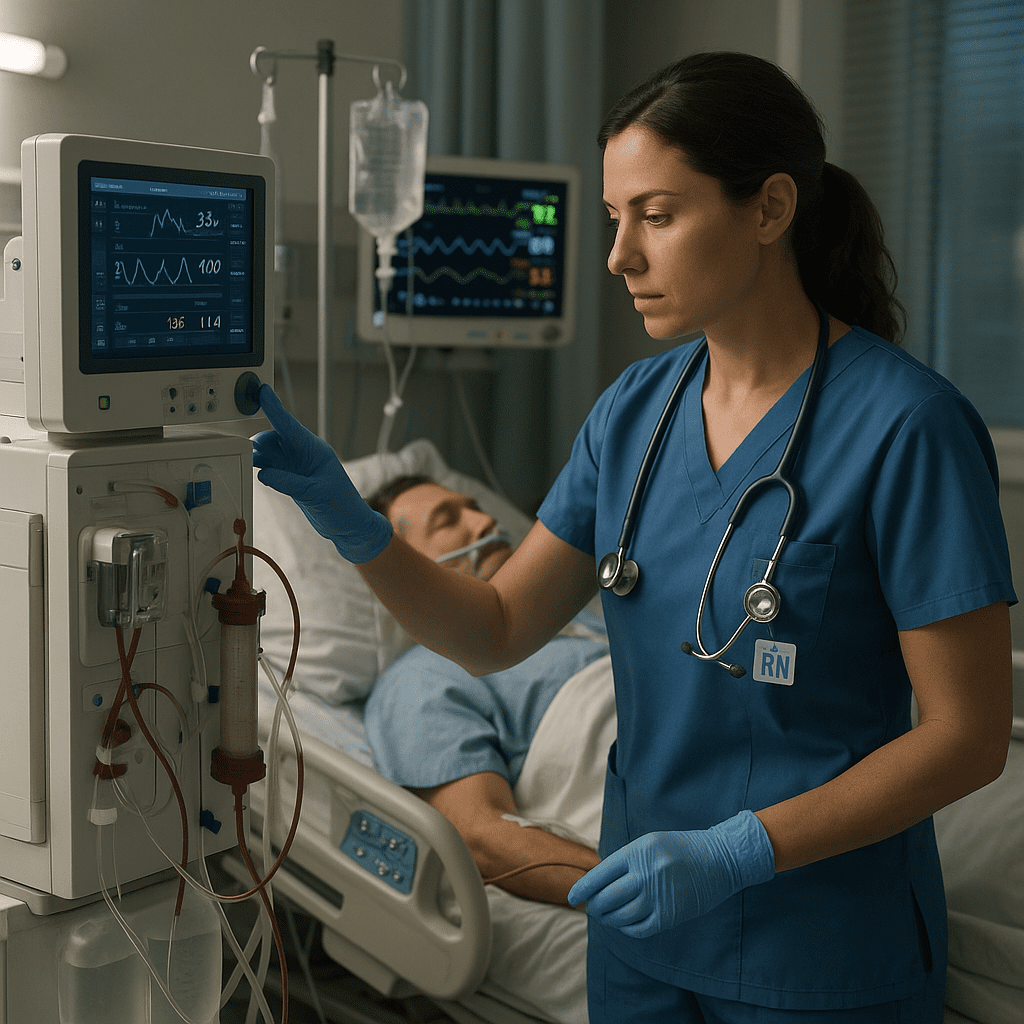
Continuous Renal Replacement Therapy (CRRT) is a lifesaving procedure commonly used in intensive care units (ICUs) to manage patients with acute kidney injury (AKI) or multi-organ failure. Every registered nurse (RN) caring for critically ill patients must understand CRRT fundamentals for safe and effective practice. This guide breaks down the essential nursing responsibilities, NCLEX concepts, and clinical priorities related to CRRT.
🧾 What is Continuous Renal Replacement Therapy (CRRT)?
CRRT is a continuous form of dialysis that gently removes fluids and wastes from the blood over 24 hours. Unlike intermittent hemodialysis, CRRT is ideal for unstable patients who cannot tolerate rapid fluid shifts.
For nurses and RN students preparing for the NCLEX, understanding CRRT helps in managing patients with severe renal dysfunction while maintaining hemodynamic stability.
⚙️ Indications for CRRT
Registered nurses should recognize key reasons a patient may need CRRT:
- Acute kidney injury (AKI) with poor urine output
- Fluid overload unresponsive to diuretics
- Electrolyte imbalances (hyperkalemia, metabolic acidosis)
- Sepsis or multi-organ dysfunction syndrome (MODS)
NCLEX tip: Always assess for rising BUN, creatinine, and potassium levels when determining renal failure severity.
💉 Types of CRRT Modalities
Nurses should be familiar with four primary CRRT modes:
- CVVH (Continuous Venovenous Hemofiltration): Removes fluid and solutes by convection.
- CVVHD (Continuous Venovenous Hemodialysis): Uses diffusion for solute clearance.
- CVVHDF (Continuous Venovenous Hemodiafiltration): Combines both convection and diffusion.
- SCUF (Slow Continuous Ultrafiltration): Removes fluid without affecting solute levels—ideal for severe fluid overload.
👩⚕️ Nursing Responsibilities in CRRT
For registered nurses, CRRT management requires continuous monitoring, critical thinking, and precise interventions. Here are key nursing responsibilities:
- Monitor Hemodynamics: Check blood pressure, heart rate, and central venous pressure regularly.
- Assess Filter Function: Look for clotting, air bubbles, or high transmembrane pressure.
- Monitor Fluid Balance: Strictly document intake and output to prevent dehydration or fluid overload.
- Check Labs Frequently: Monitor electrolytes, BUN, creatinine, and calcium.
- Ensure Machine Alarms Are Managed Promptly: Investigate causes immediately to prevent circuit loss.
- Administer Anticoagulation: Follow protocols for heparin or citrate to prevent clotting in the filter.
- Patient Education: Explain the therapy process and reassure family members.
NCLEX tip: If a CRRT alarm sounds, the nurse should first assess the patient, then troubleshoot the equipment.
💊 Common Complications and Nursing Interventions
| Complication | Nursing Intervention |
|---|---|
| Hypotension | Slow the ultrafiltration rate; administer fluids as ordered |
| Hypothermia | Use blood warmer or adjust temperature settings |
| Electrolyte imbalance | Monitor lab results; replace electrolytes per protocol |
| Circuit clotting | Flush the system or replace the filter |
| Air embolism | Stop the machine immediately and place the patient in left lateral Trendelenburg position |
🧠 NCLEX-Focused Nursing Concepts
To prepare for NCLEX, nurses should focus on:
- Safety and Infection Control: Maintain sterile technique for all connections.
- Physiological Adaptation: Recognize signs of renal failure and hemodynamic instability.
- Management of Care: Prioritize interventions and collaborate with nephrology and ICU teams.
- Pharmacological Therapies: Understand the impact of medications excreted by the kidneys.
🧩 Role of Nursing Bundles in CRRT
Implementing a nursing bundle for CRRT improves patient outcomes and ensures standardized care. These bundles may include:
- Regular circuit checks
- Electrolyte replacement protocols
- Daily filter change assessments
- Infection control measures
- Documentation audits
Using structured bundles also helps registered nurses demonstrate clinical competence—an essential skill tested in the NCLEX.
🩺 Key Takeaways for RNs and Nursing Students
- CRRT provides slow, continuous blood filtration for critically ill patients.
- RNs must closely monitor fluid balance, electrolytes, and machine performance.
- Recognizing early signs of complications can prevent serious adverse outcomes.
- Nursing bundles standardize care, enhance safety, and align with NCLEX standards.
- Patient-centered care and interdisciplinary collaboration are essential for CRRT success.
💬 Final Thoughts
As a registered nurse, mastering CRRT not only strengthens ICU competence but also reinforces core NCLEX concepts. Whether managing complex patients or studying from a nursing bundle, understanding CRRT is a crucial part of critical care nursing practice.
FAQ: Continuous Renal Replacement Therapy (CRRT) — Nursing Guide
CRRT is a continuous form of dialysis used in critically ill patients with acute kidney injury. Unlike traditional dialysis, it slowly removes waste, electrolytes, and fluids over 24 hours, making it ideal for unstable patients in the ICU.
The RN nurse monitors the CRRT machine, checks for clotting or line issues, assesses fluid balance, tracks lab results, and ensures patient safety. Registered nurses also communicate any abnormalities to the healthcare team immediately.
Nursing priorities include maintaining hemodynamic stability, monitoring electrolytes, assessing the filter and access site, and documenting fluid input and output. Nurses must also ensure correct machine settings per physician orders.
On the NCLEX exam, questions may test the nurse’s ability to identify complications such as hypotension, hypocalcemia, or clotting in the circuit. Understanding CRRT principles helps nurses choose safe, evidence-based actions.