Calcium regulation is one of the most frequently tested endocrine and electrolyte topics on the NCLEX, and for good reason. Calcium directly affects cardiac function, neuromuscular activity, blood clotting, and bone stability. For every nurse, especially the critical care registered nurse (RN nurse), understanding how parathyroid hormone (PTH) and vitamin D regulate calcium is essential for safe and effective nursing practice.
Calcium balance is not random — it is a tightly controlled hormonal process.
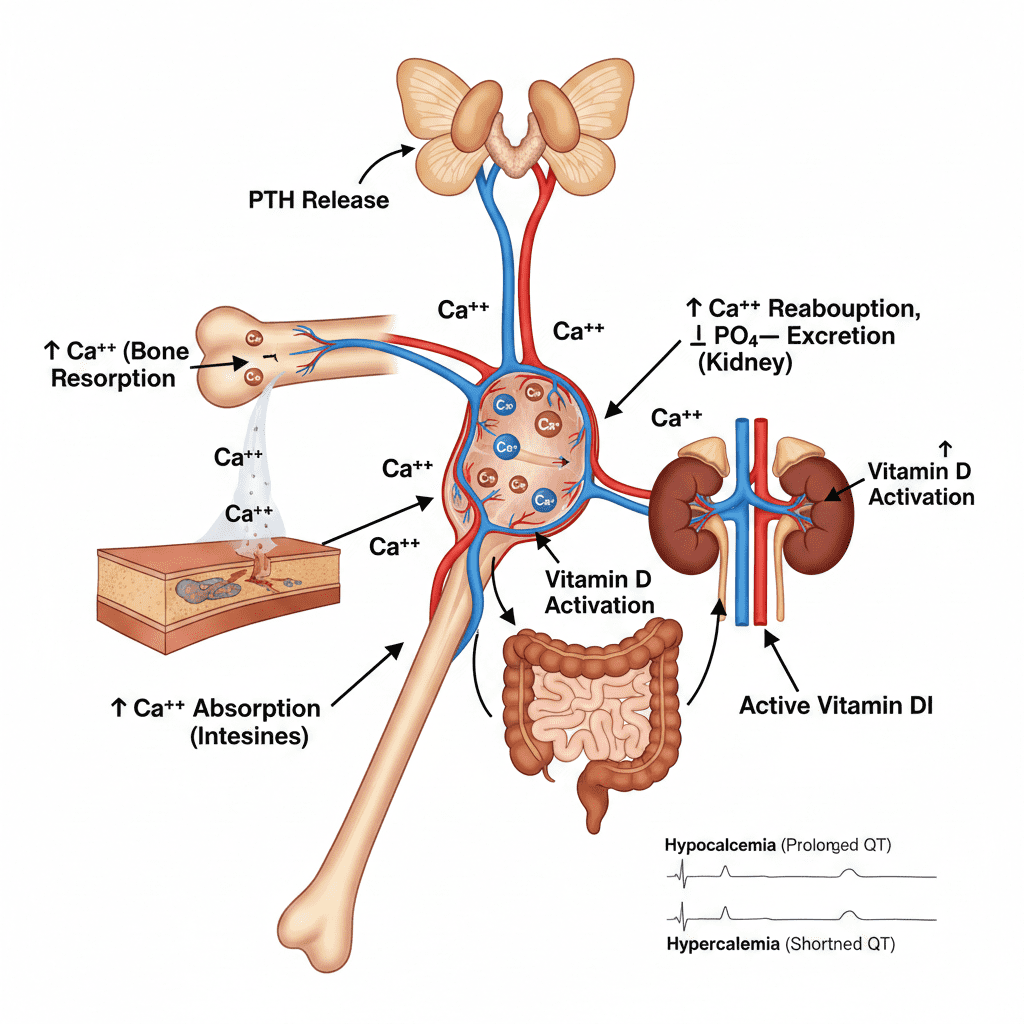
Parathyroid hormone raises serum calcium, while vitamin D enhances calcium absorption — together they maintain life-sustaining balance.
Normal Calcium Levels
Total serum calcium:
8.6–10.2 mg/dL
Ionized calcium (most clinically important):
4.6–5.3 mg/dL
The RN nurse must remember that low albumin can falsely lower total calcium levels. Always assess ionized calcium when possible.
Overview of Calcium Physiology
Calcium plays a role in:
- Cardiac contraction
- Skeletal muscle contraction
- Nerve impulse transmission
- Blood clotting
- Bone mineralization
Because calcium affects multiple body systems, imbalances can quickly become life-threatening — a major focus on the NCLEX and in acute care nursing.
Parathyroid Hormone (PTH): The Calcium Booster
Parathyroid hormone is released from the parathyroid glands in response to low serum calcium.
When Calcium Is Low:
PTH acts on three organs:
1️⃣ Bone
- Stimulates osteoclasts
- Releases calcium into bloodstream
2️⃣ Kidneys
- Increases calcium reabsorption
- Decreases phosphate reabsorption
3️⃣ Intestines (Indirectly)
- Activates vitamin D
- Enhances dietary calcium absorption
For the registered nurse, recognizing that PTH raises calcium and lowers phosphate is key.
Vitamin D: The Calcium Absorption Hormone
Vitamin D (calcitriol when active) enhances calcium absorption in the intestines.
Without adequate vitamin D:
- Dietary calcium absorption decreases
- Serum calcium falls
- PTH increases (secondary hyperparathyroidism)
This is commonly seen in:
- Chronic kidney disease
- Malnutrition
- Limited sun exposure
- Elderly patients
The RN nurse must assess both calcium and vitamin D status in at-risk patients.
Clinical Correlation: Hypocalcemia
Hypocalcemia (<8.6 mg/dL) may result from:
- Hypoparathyroidism
- Vitamin D deficiency
- Chronic kidney disease
- Acute pancreatitis
- Massive blood transfusion
Symptoms (Remember “CATS” for NCLEX)
- Convulsions
- Arrhythmias
- Tetany
- Spasms/Stridor
ECG change:
- Prolonged QT interval
The nurse must monitor for laryngospasm, which can be life-threatening.
Clinical Correlation: Hypercalcemia
Hypercalcemia (>10.2 mg/dL) is often caused by:
- Hyperparathyroidism
- Malignancy
- Excess vitamin D
- Prolonged immobilization
Symptoms (Remember “Bones, Stones, Groans, and Psychiatric Overtones”)
- Bone pain
- Kidney stones
- Abdominal pain
- Confusion
ECG change:
- Shortened QT interval
For the RN nurse, cardiac monitoring is critical.
Parathyroid Disorders in Clinical Practice
Hyperparathyroidism
Excess PTH → high calcium, low phosphate
Seen in:
- Parathyroid adenoma
- Chronic kidney disease (secondary)
Nursing priorities:
- Hydration
- Cardiac monitoring
- Fall precautions
Hypoparathyroidism
Low PTH → low calcium
Often occurs after thyroid surgery.
The registered nurse should monitor:
- Chvostek’s sign
- Trousseau’s sign
- Airway patency
These are high-yield NCLEX assessment findings.
Vitamin D and Chronic Kidney Disease
Kidneys activate vitamin D.
In renal failure:
- Vitamin D activation decreases
- Calcium absorption decreases
- PTH increases (secondary hyperparathyroidism)
- Bone demineralization occurs
The RN nurse caring for dialysis patients must understand this hormonal chain reaction.
Cardiac Effects of Calcium Imbalance
Calcium directly affects myocardial contraction.
Hypocalcemia:
- Weak contractions
- Prolonged QT
- Risk of Torsades
Hypercalcemia:
- Stronger contractions initially
- Short QT
- Risk of heart block
Electrolyte-related ECG interpretation is heavily tested on the NCLEX.
Nursing Bundle for Calcium Regulation Monitoring
A structured electrolyte nursing bundle should include:
- Monitoring serum calcium and ionized calcium
- Monitoring phosphate levels
- Assessing PTH levels when indicated
- Evaluating vitamin D status
- Continuous ECG monitoring in severe imbalances
- Assessing neuromuscular symptoms
This systematic approach improves patient safety and clinical outcomes.
Treatment Overview in Clinical Practice
Hypocalcemia Treatment:
- IV calcium gluconate (slow administration)
- Oral calcium supplements
- Vitamin D supplementation
The RN nurse must monitor cardiac rhythm during IV calcium administration.
Hypercalcemia Treatment:
- IV fluids
- Loop diuretics
- Calcitonin
- Bisphosphonates
Hydration is the priority nursing intervention.
NCLEX High-Yield Review
- PTH increases calcium
- PTH decreases phosphate
- Vitamin D increases intestinal calcium absorption
- Hypocalcemia → prolonged QT
- Hypercalcemia → shortened QT
- After thyroid surgery → monitor for hypocalcemia
If a post-thyroidectomy patient develops tingling or muscle spasms, check calcium immediately.
Integrating Hormonal Calcium Regulation into Nursing Practice
For the modern nurse and experienced RN nurse, understanding calcium regulation goes beyond memorization. It strengthens:
- Critical thinking
- ECG interpretation
- Endocrine system understanding
- Electrolyte management
- Patient education
Mastery of PTH and vitamin D regulation also improves NCLEX confidence and clinical decision-making.
Final Thoughts
Calcium regulation is a dynamic balance maintained by parathyroid hormone and vitamin D. When disrupted, cardiac, neuromuscular, and skeletal complications quickly follow.
For every registered nurse, applying a structured nursing bundle for calcium monitoring ensures early detection of imbalances and safer patient outcomes.
Because endocrine and electrolyte disorders remain a major component of the NCLEX, mastering this topic strengthens both exam readiness and real-world nursing expertise.