A High-Yield NCLEX Guide for the Nurse, Registered Nurse, and RN Nurse
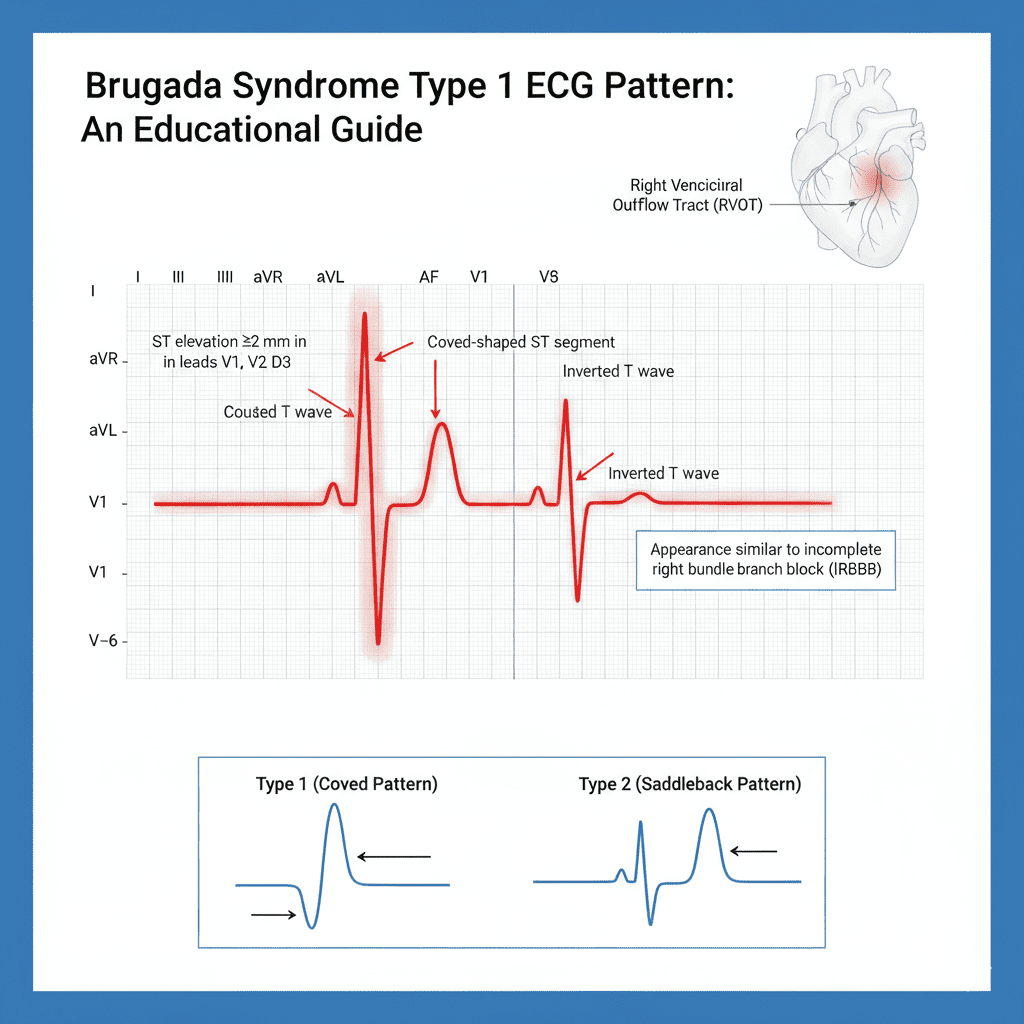
Brugada syndrome is identified on ECG by ST elevation in V1–V3 with a characteristic “coved” or “saddleback” pattern and a high risk for sudden ventricular arrhythmias.
For every nurse, registered nurse, and RN nurse, recognizing dangerous ECG patterns is critical. Brugada syndrome is one of the most important inherited arrhythmia disorders tested on the NCLEX and encountered in emergency and cardiac nursing practice.
Unlike STEMI, Brugada syndrome is not caused by coronary artery blockage — it is an electrical channelopathy that can lead to sudden cardiac death if not recognized early.
What Is Brugada Syndrome?
Brugada syndrome is a genetic sodium channel disorder that affects cardiac conduction, particularly in the right ventricular outflow tract.
It increases the risk of:
- Ventricular tachycardia (VT)
- Ventricular fibrillation (VF)
- Sudden cardiac arrest
For the registered nurse, early recognition of the ECG pattern may be lifesaving.
Where to Look on the ECG
Brugada patterns appear in:
Leads V1, V2, V3
(Right precordial leads)
These leads view the right side of the heart — the area most affected in Brugada syndrome.
The 3 Brugada ECG Patterns
Type 1 (Diagnostic Pattern)
This is the most important pattern for NCLEX and clinical practice.STElevation≥2mminV1–V3withCovedMorphologyST Elevation ≥2 mm in V1–V3 with Coved MorphologySTElevation≥2mminV1–V3withCovedMorphology
Features:
- ≥2 mm ST elevation
- Downsloping “coved” ST segment
- Inverted T wave
- Appears like a partial right bundle branch block
This pattern is diagnostic when seen with clinical criteria.
For the RN nurse, this is the pattern most associated with sudden arrhythmia risk.
Type 2 (Saddleback Pattern)
Features:
- ST elevation ≥2 mm
- Saddle-shaped ST segment
- Positive or biphasic T wave
Less specific than Type 1.
Type 3
Features:
- ST elevation <2 mm
- Coved or saddleback appearance
Not diagnostic alone.
Why Brugada Is Dangerous
Brugada syndrome predisposes patients to:
- Polymorphic ventricular tachycardia
- Ventricular fibrillation
- Sudden cardiac arrest during sleep
Many patients are young and otherwise healthy.
For the cardiac nurse, unexplained syncope plus a suspicious ECG should raise immediate concern.
Clinical Triggers Nurses Must Know
Brugada ECG changes can be unmasked or worsened by:
- Fever
- Sodium channel–blocking medications
- Electrolyte imbalances
- Cocaine
- Certain antidepressants or antiarrhythmics
In emergency nursing, always assess temperature. Fever can trigger lethal arrhythmias in these patients.
Brugada vs STEMI: Key Differences
| Feature | Brugada | STEMI |
|---|---|---|
| Cause | Genetic channelopathy | Coronary artery occlusion |
| Leads affected | V1–V3 | Varies by location |
| Reciprocal changes | No | Often present |
| Troponin elevation | No | Yes |
| Treatment | ICD placement | PCI |
This comparison is high-yield for NCLEX.
Nursing Assessment Priorities
For the registered nurse or RN nurse:
- Assess for history of syncope
- Ask about family history of sudden cardiac death
- Monitor for ventricular dysrhythmias
- Check for fever
- Continuous cardiac monitoring
Nursing Bundle for Suspected Brugada Syndrome
A structured cardiac nursing bundle may include:
- Continuous ECG monitoring
- Immediate provider notification
- Temperature management (aggressive fever control)
- Electrolyte correction
- Avoidance of contraindicated medications
- Defibrillator readiness
In high-risk patients, implantable cardioverter-defibrillator (ICD) placement is the definitive treatment.
There is no medication that cures Brugada syndrome.
NCLEX Pearls for Brugada Syndrome
✔️ ST elevation in V1–V3 without MI
✔️ Coved ST segment = Type 1 (diagnostic)
✔️ Fever can trigger arrhythmia
✔️ Sudden cardiac death risk in young adults
✔️ ICD is treatment of choice
The NCLEX often tests recognition of right precordial ST elevation without reciprocal changes.
Red Flags Every Nurse Should Recognize
Immediate escalation if:
- Syncope with abnormal ECG
- Ventricular tachycardia on monitor
- Family history of unexplained sudden death
- Fever with Brugada pattern
For the practicing nurse, rapid recognition can prevent cardiac arrest.
Advanced Clinical Insight for the RN Nurse
Brugada syndrome can mimic:
- Anterior STEMI
- Right bundle branch block
- Early repolarization
Key distinction:
Brugada does not produce evolving changes like MI.
Experienced cardiac nursing professionals correlate ECG findings with clinical presentation and labs.
Final Thoughts for the Nurse and Registered Nurse
Brugada syndrome is a silent but deadly electrical disorder.
Recognizing the ECG pattern:
- Prevents misdiagnosis
- Avoids inappropriate STEMI activation
- Reduces risk of sudden cardiac arrest
- Strengthens critical thinking for NCLEX
For every RN nurse, mastering high-risk ECG patterns is part of advanced cardiac nursing competency.
When you see ST elevation in V1–V3 —
Ask yourself:
Is this a STEMI…
Or is this Brugada?
Because the treatment pathway is very different —
And recognizing the difference saves lives.