In the fast-paced world of bedside care, recognizing life-threatening cardiac rhythms quickly can save lives. Although you don’t need to be a cardiologist, you must know how to spot critical arrhythmias on a monitor or EKG strip — and understand the next steps.
This guide breaks down the Big 5 — the deadliest heart rhythms every nurse should master.
❤️ Why These Rhythms Matter
Some arrhythmias can stop the heart from pumping effectively, causing cardiac arrest within seconds or minutes. By knowing them, you can call a code, grab the crash cart, start CPR, and assist the team in delivering the right treatment without delay.
⚡ The Big 5 Life-Threatening Rhythms
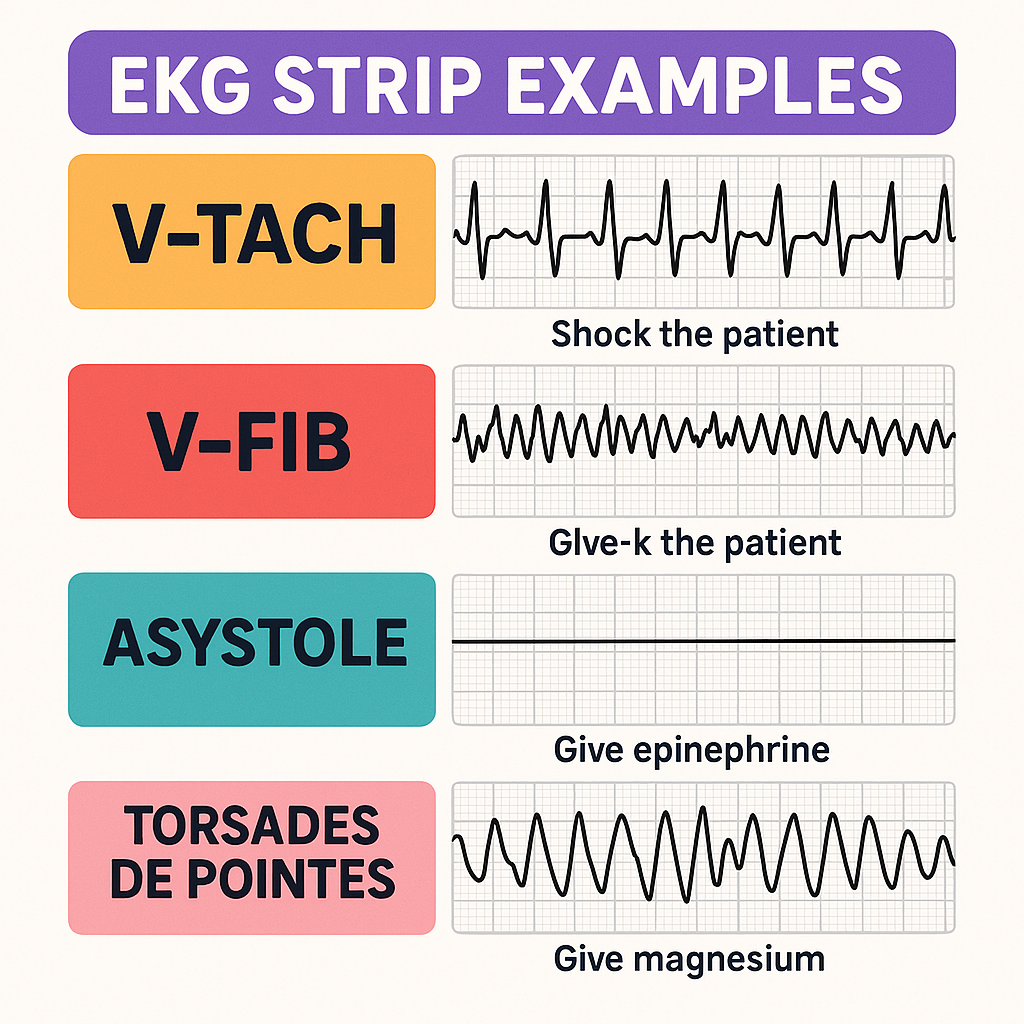
✅ 1. Ventricular Tachycardia (V-Tach)
✅ 2. Ventricular Fibrillation (V-Fib)
✅ 3. Asystole
✅ 4. Pulseless Electrical Activity (PEA)
✅ 5. Torsades de Pointes
Let’s explore each one in plain language.
1️⃣ Ventricular Tachycardia (V-Tach)
What it is:
V-Tach occurs when the ventricles fire off fast electrical signals independently. This overrides the normal pacemaker and may pump blood so poorly that the patient has no pulse.
EKG appearance:
- Wide, regular QRS complexes
- Rate often 150–250 bpm
- Consistent “big hills” on the strip
Patient check:
- With pulse: May cause dizziness, hypotension
- Pulseless: Treat like V-Fib — Code Blue
Nursing action:
- Stable with pulse: Call provider, prepare antiarrhythmics (like amiodarone), consider synchronized cardioversion
- Unstable or pulseless: Start CPR immediately, defibrillate, follow ACLS
2️⃣ Ventricular Fibrillation (V-Fib)
What it is:
This is total electrical chaos. The ventricles quiver instead of contracting, so no blood is pumped. Rapid action is essential — the patient is clinically dead without intervention.
EKG appearance:
- No P waves or QRS complexes
- Chaotic, squiggly baseline
Nursing action:
- Call Code Blue immediately
- Start CPR
- Defibrillate ASAP
- Administer epinephrine and follow ACLS
3️⃣ Asystole
What it is:
Asystole is a flatline — no electrical activity, no heartbeat, no blood flow. This represents true cardiac arrest.
EKG appearance:
- Flat line (check all leads to ensure it’s not a loose lead)
Nursing action:
- Call Code Blue
- Start CPR immediately
- Do NOT shock — no electrical activity is present
- Give epinephrine and identify reversible causes (H’s and T’s)
4️⃣ Pulseless Electrical Activity (PEA)
What it is:
The monitor may show a rhythm, but there is no pulse. The heart’s electrical system works, yet the muscle cannot pump effectively.
EKG appearance:
- Can mimic normal sinus rhythm, bradycardia, or other organized rhythms — but no pulse
Nursing action:
- Call Code Blue
- Start CPR immediately
- Do NOT shock
- Give epinephrine and identify causes:
- H’s: Hypoxia, hypovolemia, hydrogen ion (acidosis), hyper/hypokalemia, hypothermia
- T’s: Tension pneumothorax, tamponade, toxins, thrombosis (MI, PE)
5️⃣ Torsades de Pointes
What it is:
A special type of V-Tach with twisting peaks. Often linked to low magnesium or prolonged QT interval, it can suddenly degenerate into V-Fib.
EKG appearance:
- Polymorphic V-Tach: QRS complexes twist around the baseline like a ribbon or spindle
Nursing action:
- If unstable: Defibrillate immediately
- Give IV magnesium sulfate
- Correct low potassium
- Stop QT-prolonging medications (some antibiotics, antiarrhythmics)
🗝️ Quick Rhythm Comparison
| Rhythm | Pulse? | Shockable? | What to Do |
|---|---|---|---|
| V-Tach (pulseless) | ❌ No | ✅ Yes | CPR + Defibrillation |
| V-Fib | ❌ No | ✅ Yes | CPR + Defibrillation |
| Asystole | ❌ No | ❌ No | CPR + Epi + Fix causes |
| PEA | ❌ No | ❌ No | CPR + Epi + Fix causes |
| Torsades | ❌ No / unstable | ✅ Yes | CPR + Defib + Magnesium |
✅ How to Master These Rhythms
- Always check the patient first: Monitors do not confirm a pulse
- Memorize key patterns: Wide QRS = V-Tach, squiggly = V-Fib, flat = Asystole, normal rhythm with no pulse = PEA
- Know what to do: Shockable? Defibrillate. Not shockable? CPR, epinephrine, fix causes
- Practice ACLS: Regular mock codes, reading strips, and team drills improve confidence
❤️ Nurse’s Role in a Code
During cardiac arrest, every second counts. Nurses should:
- Call the code immediately
- Start high-quality CPR
- Grab the crash cart and attach defibrillator pads
- Know key meds (epinephrine, amiodarone, magnesium)
- Communicate clearly with the code leader
Confidence comes with practice. Use simulation labs and review strips often.
🎓 Key Takeaways
- V-Tach & V-Fib: Defibrillate
- Asystole & PEA: CPR, epi, fix cause — no shock
- Torsades: Magnesium + defib if unstable
Stay calm, focused, and trust your training — you are your patient’s best chance for survival.