Acute Respiratory Distress Syndrome (ARDS) is one of the most critical respiratory conditions that every registered nurse (RN nurse) must understand. It’s not only a frequent cause of ICU admissions but also a high-yield topic on the NCLEX. For nursing students and practicing nurses, ARDS can seem overwhelming — but when broken down into simple concepts, it becomes much easier to manage and remember.
This guide will walk you through what ARDS is, its causes, nursing priorities, and simplified NCLEX-focused notes, so you can approach this condition with confidence.
🌬️ What is ARDS?
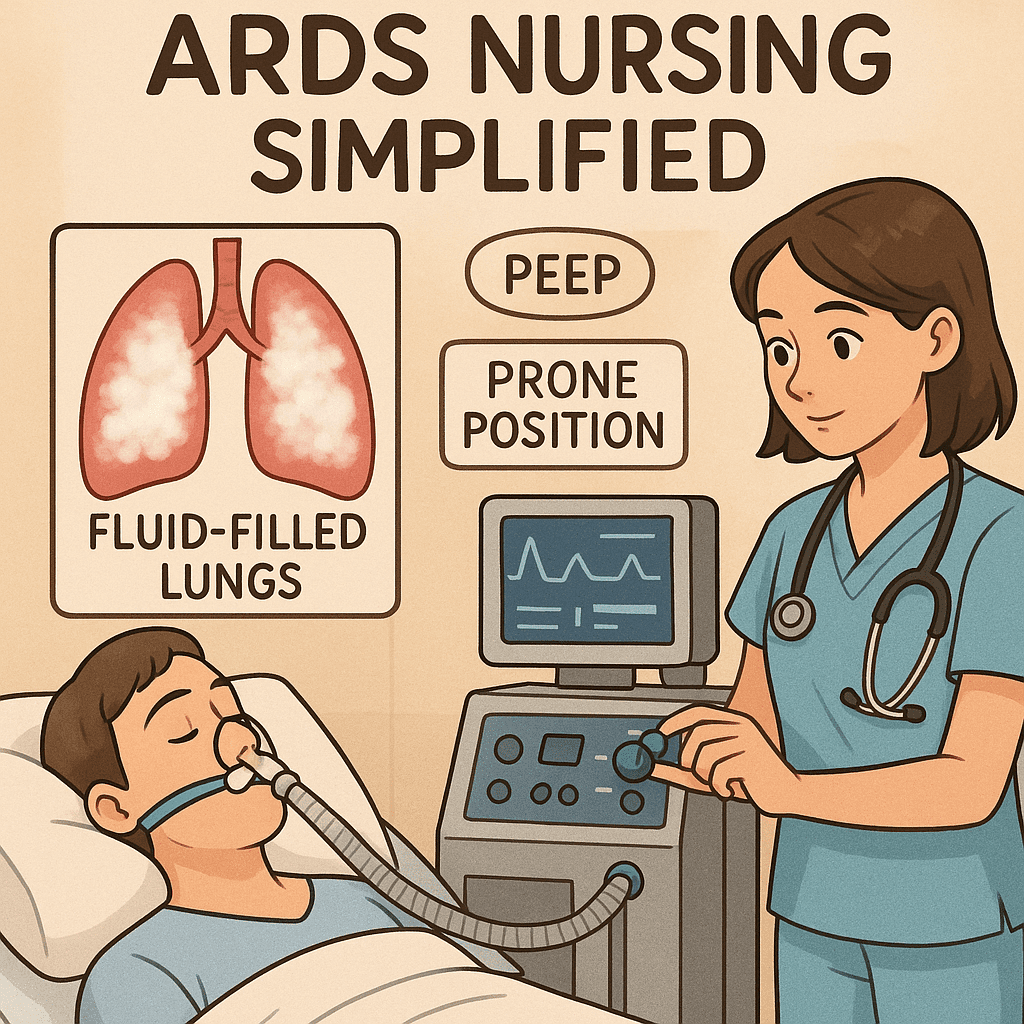
ARDS is a life-threatening condition where fluid leaks into the alveoli, preventing oxygen from moving into the bloodstream. It leads to severe hypoxemia (low blood oxygen), even when oxygen is given.
- Key problem: The alveoli are filled with fluid instead of air.
- Result: The patient can’t get enough oxygen, no matter how much they breathe in.
🔍 Causes of ARDS (Common NCLEX Triggers)
ARDS usually develops after another severe illness or injury. The most common causes include:
- Sepsis (most common cause)
- Aspiration (inhaled stomach contents)
- Pneumonia
- Trauma (chest injuries, burns, near drowning)
- Massive blood transfusions
👉 Think: “S.A.P.T.M” → Sepsis, Aspiration, Pneumonia, Trauma, Massive transfusion.
🩺 Signs & Symptoms (What the RN Nurse Sees)
- Severe shortness of breath (even with oxygen)
- Low oxygen saturation (SpO₂) despite high O₂ delivery
- Crackles in the lungs (fluid)
- Tachypnea and tachycardia
- Restlessness, confusion (low oxygen to the brain)
On chest X-ray: “white-out lung” appearance (due to fluid-filled alveoli).
⚡ Nursing Priorities in ARDS
ARDS requires fast, organized nursing care. Here’s what every nurse must focus on:
1. Oxygenation & Ventilation
- Patients usually need mechanical ventilation.
- PEEP (Positive End-Expiratory Pressure) is key: it keeps alveoli open and improves oxygenation.
- Monitor SpO₂ and ABGs (arterial blood gases).
2. Positioning
- Prone positioning (lying on the stomach) improves oxygenation by opening up lung fields.
- Rotate positions to prevent skin breakdown.
3. Fluid Balance
- Be cautious with IV fluids (too much fluid worsens ARDS).
- Monitor urine output and daily weights.
4. Medications
- Diuretics → reduce fluid overload.
- Vasopressors → support blood pressure if shock is present.
- Antibiotics → if infection (like sepsis or pneumonia) is the trigger.
5. Supportive Nursing Care
- Maintain airway and suction if needed.
- Reduce anxiety (calm environment, sedation if ventilated).
- Provide family teaching and emotional support.
📝 NCLEX Nursing Notes for ARDS
- PEEP improves oxygenation but can cause barotrauma (watch for pneumothorax).
- Prone positioning = improved survival.
- If oxygen doesn’t improve despite high O₂ → think ARDS.
- Always monitor for complications: ventilator-associated pneumonia (VAP), multi-organ failure.
📦 How Nursing Bundles Can Help
Studying ARDS alongside other critical care topics in a nursing bundle allows students and RN nurses to see the bigger picture of ICU care. Bundles often include:
- EKG rhythms
- Respiratory emergencies
- Shock management
- Sepsis care
These resources help nursing students prepare for NCLEX questions and apply safe practice at the bedside.
✅ Key Takeaway
ARDS is a life-threatening lung condition that demands quick recognition and skilled nursing interventions. For the registered nurse, understanding the basics — causes, symptoms, and nursing priorities — is essential both for passing the NCLEX and for saving lives in practice.
❓ FAQs on ARDS Nursing Simplified
ARDS stands for Acute Respiratory Distress Syndrome. It is a severe lung condition where the alveoli fill with fluid, preventing proper oxygen exchange. For a nurse or RN nurse, early recognition and supportive interventions are critical.
The top priorities include:
Maintaining adequate oxygenation (high-flow O₂ or mechanical ventilation).
Positioning the patient prone to improve oxygen exchange.
Monitoring vital signs, ABGs, and pulse oximetry.
Supporting hemodynamics with fluids and medications as needed.
Common causes include sepsis, trauma, pneumonia, pancreatitis, aspiration, and severe COVID-19 infection. NCLEX questions often highlight sepsis and aspiration as key triggers.
Watch for increasing shortness of breath, refractory hypoxemia (low oxygen not improving with O₂ therapy), rapid breathing, crackles in the lungs, and chest X-ray showing “white-out” lungs.
PEEP (Positive End-Expiratory Pressure) helps keep alveoli open during exhalation, improving oxygenation. Nurses must monitor for barotrauma and decreased blood pressure when PEEP is high.
The NCLEX often asks about recognizing early symptoms, prioritizing interventions (like positioning and oxygen therapy), and understanding ventilator settings such as PEEP.