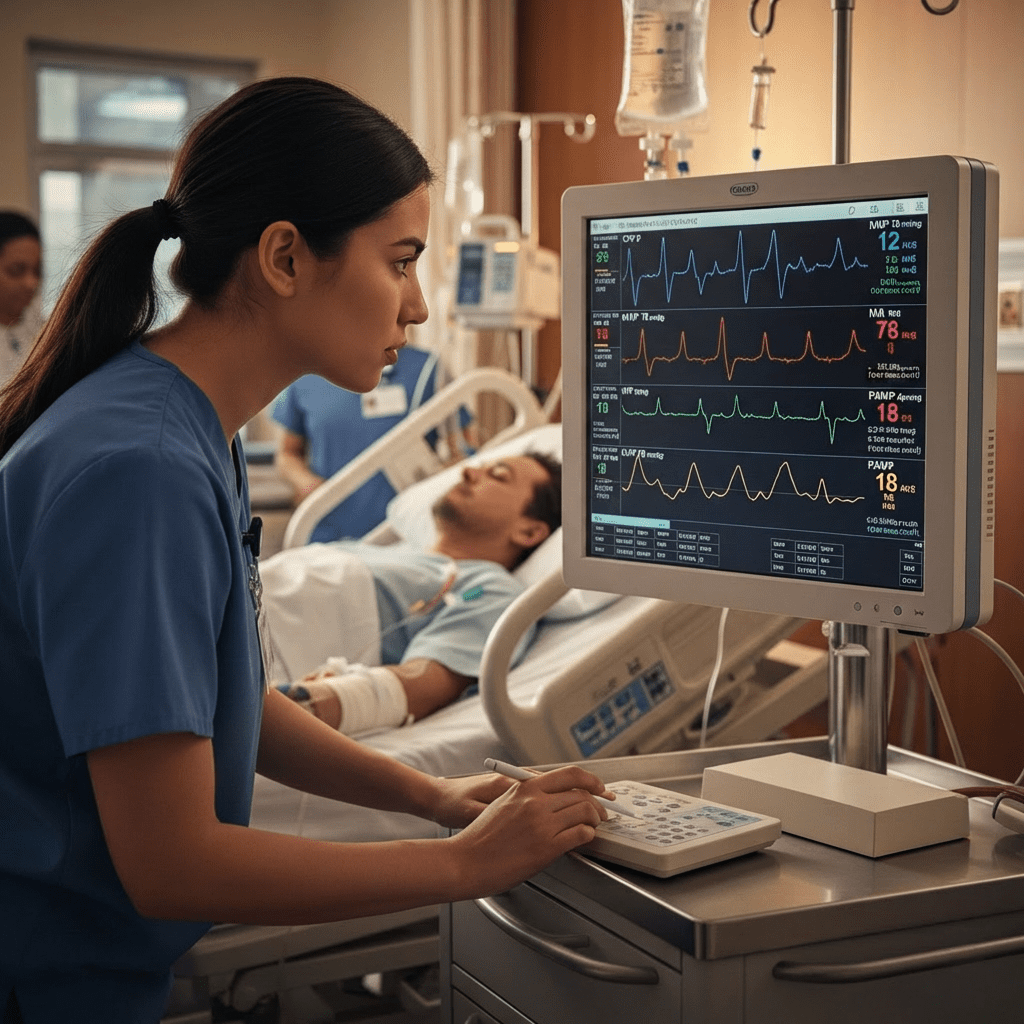
Advanced hemodynamic monitoring is a core skill for every ICU nurse and an important concept tested on the NCLEX. In critical care settings, understanding values such as CVP, MAP, SVR, and PAWP allows the registered nurse (RN nurse) to detect shock early, guide fluid therapy, and evaluate medication effects.
Although these numbers may look complex at first, clinical interpretation becomes much easier when nursing students understand what each value truly represents inside the patient’s body. Therefore, this guide explains advanced hemodynamic monitoring in a simple, clinical way that supports both real bedside nursing and NCLEX success.
Why Advanced Hemodynamic Monitoring Matters in Nursing
Critically ill patients often experience rapid cardiovascular changes. Because of this instability, continuous monitoring helps the nurse recognize deterioration before it becomes life-threatening.
Hemodynamic values help answer key clinical questions:
- Is the patient fluid overloaded or dehydrated?
- Is blood pressure adequate for organ perfusion?
- Is the heart pumping effectively?
- Are blood vessels too constricted or too dilated?
For NCLEX preparation, remember that hemodynamic monitoring is closely linked to shock states, heart failure, sepsis, and critical care nursing—all high-yield exam topics often included in a comprehensive nursing bundle.
Understanding Mean Arterial Pressure (MAP)
What Is MAP?
Mean Arterial Pressure (MAP) reflects the average pressure in the arteries during one cardiac cycle. In simple terms, it shows whether organs are receiving enough blood flow.
Normal MAP:
70–100 mmHg
A MAP below 65 mmHg is generally considered inadequate for organ perfusion.
Why MAP Is Clinically Important
MAP is one of the most important numbers in ICU nursing practice. Physicians frequently write orders such as:
“Maintain MAP above 65 mmHg.”
If MAP drops, organs such as the kidneys and brain may not receive enough oxygenated blood. Consequently, the RN nurse must act quickly.
Nursing Interpretation of MAP
Low MAP may indicate:
- Hypovolemia
- Cardiogenic shock
- Septic shock
- Hemorrhage
High MAP may indicate:
- Hypertension
- Vasoconstriction
- Excess vasopressor use
From an NCLEX perspective, if MAP is low, the nurse should assess:
- Volume status
- Cardiac output
- Need for fluids or vasopressors
Central Venous Pressure (CVP)
What Is CVP?
Central Venous Pressure (CVP) measures pressure in the right atrium. It reflects right-sided heart function and fluid status.
Normal CVP:
2–6 mmHg
Clinical Meaning of CVP
CVP helps determine whether the patient needs fluids or diuretics.
Low CVP may indicate:
- Dehydration
- Blood loss
- Vasodilation (sepsis)
High CVP may indicate:
- Fluid overload
- Right-sided heart failure
- Pulmonary hypertension
However, CVP must never be interpreted alone. Instead, the nurse should assess the entire clinical picture, including urine output, blood pressure, and lung sounds.
On the NCLEX, remember:
Low CVP + Low BP → Think hypovolemia first.
Systemic Vascular Resistance (SVR)
What Is SVR?
Systemic Vascular Resistance (SVR) measures the resistance the left ventricle must overcome to pump blood through systemic circulation.
Normal SVR:
800–1200 dynes/sec/cm⁵
Clinical Interpretation of SVR
High SVR means vessels are constricted.
Causes of high SVR:
- Hypovolemic shock
- Cardiogenic shock
- Cold extremities
Low SVR means vessels are dilated.
Causes of low SVR:
- Septic shock
- Anaphylaxis
- Neurogenic shock
For example, in septic shock, SVR is typically low due to widespread vasodilation. Therefore, vasopressors like norepinephrine are often administered to increase vascular tone.
For the registered nurse, recognizing SVR patterns is essential when titrating vasopressors—an advanced skill frequently included in critical care nursing bundles.
Pulmonary Artery Wedge Pressure (PAWP)
What Is PAWP?
Pulmonary Artery Wedge Pressure (PAWP), also called pulmonary capillary wedge pressure, estimates left atrial pressure. It reflects left ventricular preload.
Normal PAWP:
6–12 mmHg
Clinical Meaning of PAWP
Low PAWP may indicate:
- Hypovolemia
- Dehydration
High PAWP may indicate:
- Left-sided heart failure
- Pulmonary edema
- Fluid overload
If PAWP is elevated and lung sounds reveal crackles, the nurse should suspect pulmonary congestion. Consequently, diuretics may be required.
For NCLEX scenarios, elevated PAWP often appears in heart failure questions.
Putting It All Together: Shock Patterns
Advanced hemodynamic interpretation becomes easier when patterns are recognized.
Hypovolemic Shock
- CVP ↓
- MAP ↓
- SVR ↑
- PAWP ↓
Treatment: Fluids
Cardiogenic Shock
- CVP ↑
- MAP ↓
- SVR ↑
- PAWP ↑
Treatment: Inotropes, cautious fluids
Septic Shock (Early)
- CVP ↓ or normal
- MAP ↓
- SVR ↓
- PAWP ↓
Treatment: Fluids + vasopressors
Recognizing these patterns is a high-level nursing skill and frequently tested on the NCLEX.
Nursing Responsibilities in Advanced Hemodynamic Monitoring
The RN nurse plays a critical role in:
- Leveling and zeroing transducers
- Ensuring waveform accuracy
- Monitoring trends, not just single values
- Assessing patient response to interventions
- Reporting significant changes promptly
Moreover, accurate documentation is essential in critical care nursing practice.
Common Mistakes in Interpretation
Even experienced nurses can make errors when interpreting hemodynamic values.
Common mistakes include:
- Treating numbers without assessing the patient
- Ignoring trends
- Failing to correlate lab values
- Over-relying on CVP alone
For NCLEX success, always choose the answer that includes patient assessment and safety.
How a Nursing Bundle Can Help
Advanced hemodynamics can feel overwhelming. However, a structured nursing bundle simplifies concepts by organizing them into:
- Normal ranges
- Clinical meaning
- Shock patterns
- NCLEX-style practice questions
Many registered nurses preparing for critical care roles or exams use hemodynamic-focused nursing bundles to strengthen understanding and confidence.
Final Clinical Tips for NCLEX and Practice
- MAP below 65 mmHg = organ perfusion risk
- Low CVP usually means low volume
- Low SVR often indicates septic shock
- High PAWP often indicates left-sided heart failure
Above all, remember that hemodynamic values must always be interpreted within the full clinical context.
Conclusion
Advanced hemodynamic monitoring is an essential competency for every ICU nurse and an important topic for the NCLEX. By understanding CVP, MAP, SVR, and PAWP clinically—not just numerically—the registered nurse can detect shock early, guide therapy safely, and improve patient outcomes.
With consistent study, real-case application, and support from a comprehensive nursing bundle, complex hemodynamic data becomes manageable and clinically meaningful for every RN nurse in critical care nursing practice.