A Clinical ECG Guide for the Nurse, Registered Nurse, and RN Nurse Preparing for NCLEX
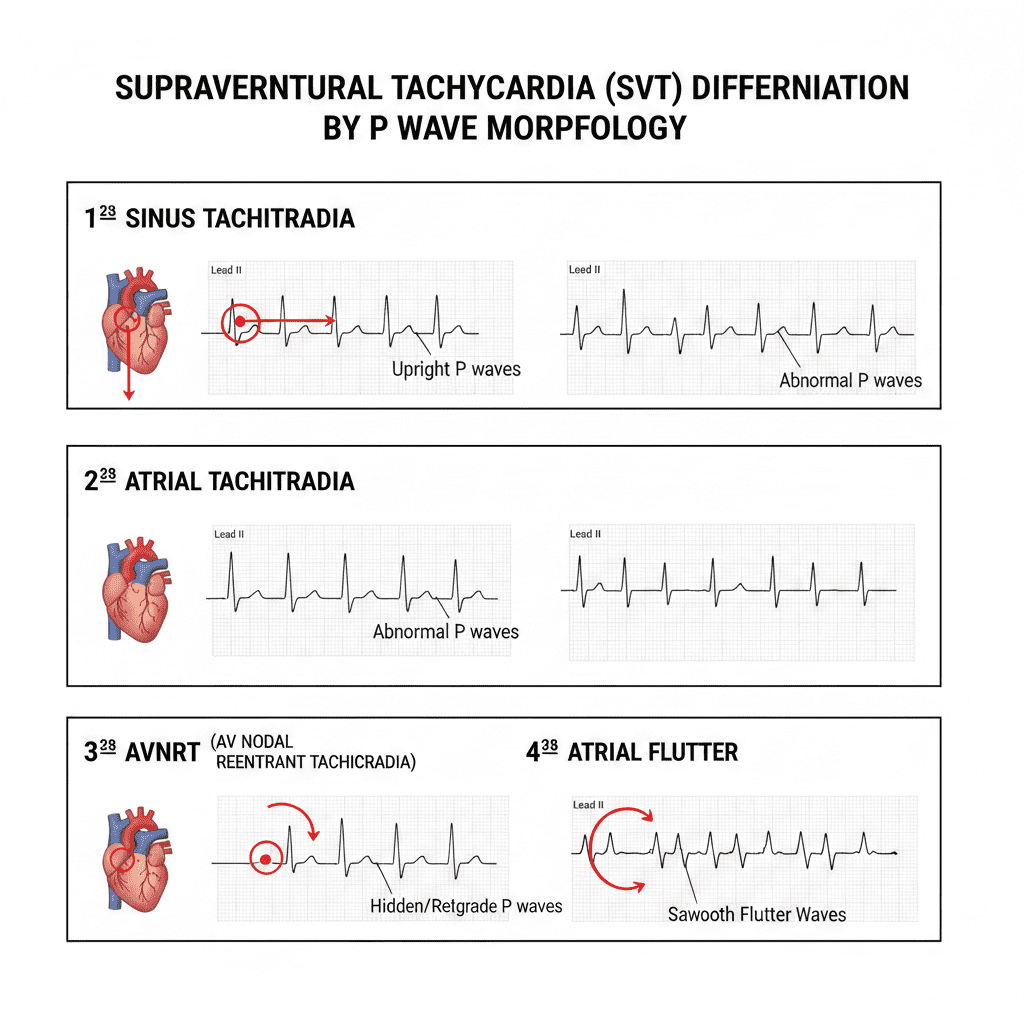
P wave morphology is the key to distinguishing types of SVT—especially when the rhythm is narrow-complex and fast.
Supraventricular tachycardia (SVT) is a broad term that describes tachycardias originating above the ventricles. For the nurse, registered nurse, and RN nurse, differentiating SVT types is critical for safe intervention, accurate documentation, and strong NCLEX performance.
Many SVTs look similar at first glance — narrow QRS, fast rate, regular rhythm. But the P wave morphology often tells the real story.
Understanding these subtle differences elevates your cardiac nursing bundle from basic rhythm recognition to advanced interpretation.
What Is SVT?
SVT typically presents as: HeartRateinSVT:150–250bpm(regular,narrowQRS)Heart Rate in SVT: 150–250 bpm (regular, narrow QRS)HeartRateinSVT:150–250bpm(regular,narrowQRS)
Characteristics:
- Narrow QRS (<0.12 sec)
- Regular rhythm (usually)
- Sudden onset and termination
- Origin above the ventricles
However, not all SVTs are the same.
Why P Waves Matter in Nursing Practice
The P wave represents atrial depolarization.
By analyzing:
- Presence or absence
- Shape (upright, inverted, abnormal)
- Relationship to QRS
- Timing
A registered nurse can identify the underlying mechanism.
This is high-yield NCLEX ECG content.
1️⃣ Sinus Tachycardia
P Wave Characteristics:
- Upright in Lead II
- Uniform shape
- One P wave before every QRS
- Normal PR interval
Clinical Clues:
- Pain
- Fever
- Hypovolemia
- Anxiety
- Sepsis
For the bedside nurse, sinus tachycardia is usually a physiologic response — not a primary rhythm disorder.
In a cardiac nursing bundle, always treat the cause.
2️⃣ Atrial Tachycardia
P Wave Characteristics:
- Abnormal P wave shape
- May be upright, flat, or peaked
- Visible before each QRS
- PR interval may vary
Why It Happens:
- Irritable atrial focus
- Digoxin toxicity
- Structural heart disease
For the RN nurse, atrial tachycardia often suggests atrial irritability.
Unlike sinus tachycardia, the P waves do not look “normal.”
3️⃣ AV Nodal Reentrant Tachycardia (AVNRT)
This is one of the most common types of paroxysmal SVT.
P Wave Characteristics:
- Often hidden within QRS
- May appear as small pseudo R’ in V1
- Or small inverted deflection after QRS
The atria and ventricles depolarize almost simultaneously.
Clinical Clues:
- Sudden onset
- Palpitations
- Young, otherwise healthy patients
For the registered nurse, absence of visible P waves in a narrow, regular tachycardia strongly suggests AVNRT.
This distinction is frequently tested on the NCLEX.
4️⃣ AV Reentrant Tachycardia (AVRT – e.g., WPW)
P Wave Characteristics:
- Retrograde P waves
- Inverted P waves after QRS
- Short RP interval
Occurs due to an accessory pathway.
If Wolff-Parkinson-White (WPW) is present in sinus rhythm:
- Short PR interval
- Delta wave
For the ICU nurse, identifying AVRT is critical before administering certain medications.
5️⃣ Atrial Flutter
Although sometimes grouped separately, atrial flutter is technically a supraventricular tachycardia.
Atrial Rate:
AtrialFlutterRate:250–350bpm(sawtoothwaves)Atrial Flutter Rate: 250–350 bpm (sawtooth waves)AtrialFlutterRate:250–350bpm(sawtoothwaves)
P Wave Characteristics:
- No true P waves
- Sawtooth “flutter waves”
- Best seen in inferior leads
Common conduction ratios:
- 2:1 → ventricular rate ~150
- 3:1 → ventricular rate ~100
For the RN nurse, a regular tachycardia at 150 bpm should always raise suspicion for 2:1 atrial flutter.
6️⃣ Atrial Fibrillation (for Comparison)
Though irregular, it’s important for differentiation.
P Wave Characteristics:
- No discernible P waves
- Chaotic baseline
- Irregularly irregular rhythm
For the nurse, the key difference from other SVTs is irregularity.
Step-by-Step Nursing Bundle for SVT Identification
- Assess patient stability first
- Determine QRS width
- Check rhythm regularity
- Look closely for P waves
- Evaluate P wave morphology
- Analyze P-to-QRS relationship
This systematic nursing bundle strengthens ECG confidence in both acute care and telemetry settings.
Clinical Significance for the Registered Nurse
Correct identification impacts:
- Medication choice (adenosine vs beta blockers)
- Cardioversion decisions
- Anticoagulation considerations
- Escalation to cardiology
For example:
- AVNRT → Often responds to vagal maneuvers
- Atrial flutter → May require anticoagulation
- Atrial tachycardia → Treat underlying cause
The experienced RN nurse understands rhythm drives treatment.
High-Yield NCLEX Pearls
✔️ Narrow QRS + no visible P waves → Think AVNRT
✔️ Abnormal P wave before each QRS → Think atrial tachycardia
✔️ Sawtooth waves → Atrial flutter
✔️ Irregular rhythm without P waves → Atrial fibrillation
✔️ Sinus tachycardia always has normal P waves
On the NCLEX, ECG questions often test pattern recognition using P wave clues.
Advanced Clinical Insight
P wave morphology reflects atrial origin:
- Upright in Lead II → Sinus origin
- Inverted in inferior leads → Retrograde activation
- Absent → Simultaneous depolarization or chaotic activity
For the modern nurse, ECG interpretation is not about memorization — it’s about pattern recognition supported by physiology.
Final Thoughts for the Nurse and RN Nurse
Differentiating SVT types using P wave morphology transforms rhythm interpretation from guessing to clinical reasoning.
When the heart rate is fast and narrow:
Don’t just count.
Look for the P wave.
Its shape, timing, and presence tell the story.
For NCLEX success and real-world cardiac nursing, mastering P wave analysis builds the confidence every registered nurse needs in high-acuity care.