A Critical Care Guide for the Nurse and Registered Nurse Preparing for NCLEX
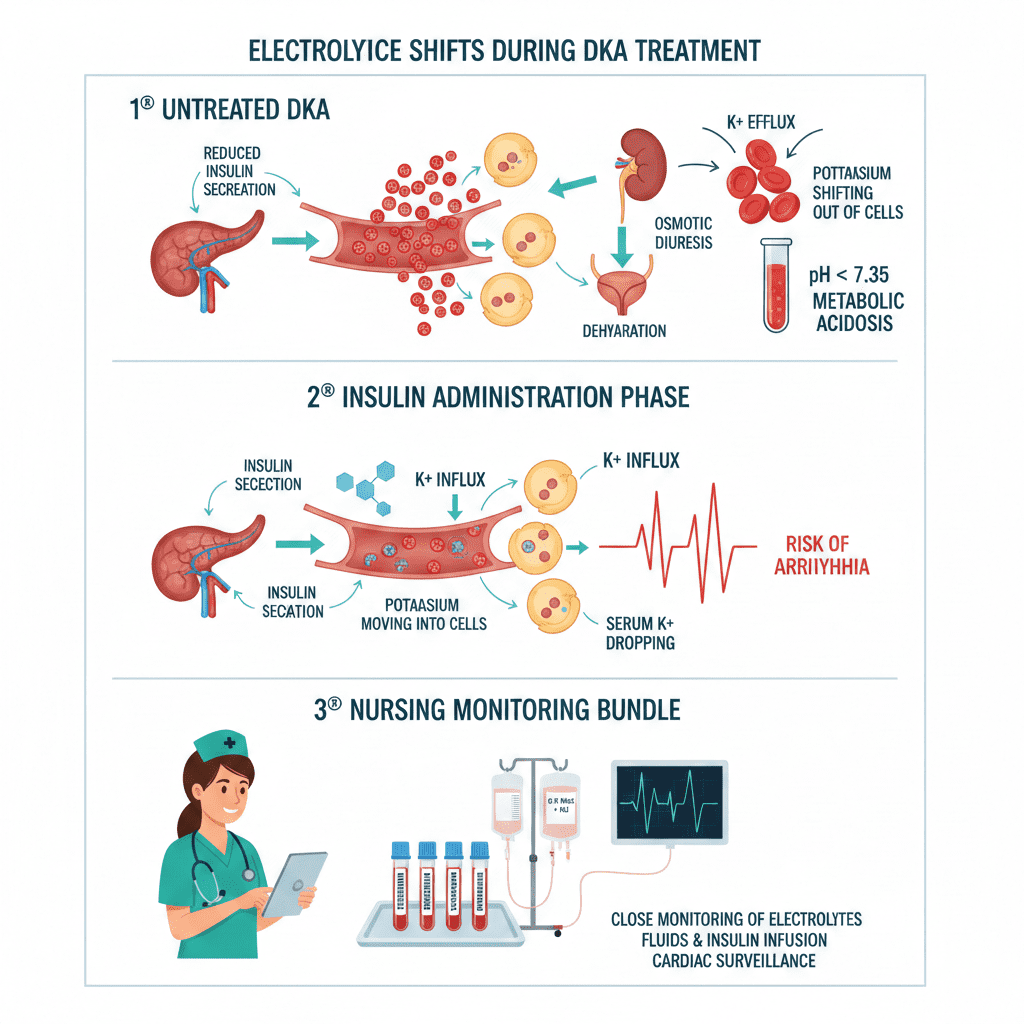
Electrolyte shifts during DKA treatment can be more dangerous than the acidosis itself—especially rapid potassium drops after insulin administration.
Diabetic ketoacidosis (DKA) is not just a glucose problem — it is a life-threatening electrolyte crisis. For the nurse, registered nurse, and RN nurse managing critically ill patients, understanding electrolyte shifts during treatment is essential for safe outcomes and strong NCLEX preparation.
DKA treatment follows a structured nursing bundle:
- Fluid resuscitation
- Insulin infusion
- Electrolyte correction
- Frequent laboratory monitoring
However, as glucose falls and insulin is administered, electrolytes shift dramatically. Let’s break down what every nursing professional must know.
Why Electrolytes Shift in DKA
DKA is caused by insulin deficiency and counter-regulatory hormone excess. This leads to:
- Hyperglycemia
- Osmotic diuresis
- Severe dehydration
- Metabolic acidosis
- Total body electrolyte depletion
Even when serum levels appear “normal,” total body stores are often critically low.
1️⃣ Potassium: The Most Dangerous Shift
What Happens in DKA?
Before treatment:
- Serum potassium may appear normal or high.
- Acidosis causes hydrogen ions to move into cells.
- Potassium shifts out of cells into bloodstream.
- But total body potassium is depleted from urinary losses.
During insulin treatment:
- Insulin drives potassium back into cells.
- Serum potassium can plummet rapidly.
- Risk: ventricular arrhythmias and cardiac arrest.
Clinical Nursing Monitoring
For the ICU nurse or RN nurse, potassium monitoring is non-negotiable.
| Potassium Level | Nursing Action |
|---|---|
| >5.2 mEq/L | Do not give potassium yet; monitor closely |
| 3.3–5.2 mEq/L | Add potassium to IV fluids |
| <3.3 mEq/L | HOLD insulin and replace potassium first |
Nursing Priority:
Never start insulin if potassium is below 3.3 mEq/L.
This is a high-yield NCLEX concept.
2️⃣ Sodium: The Corrected Sodium Concept
Hyperglycemia causes dilutional hyponatremia due to osmotic water shifts.
To evaluate true sodium status, nurses use corrected sodium: CorrectedNa=MeasuredNa+1.6×[(Glucose−100)/100]Corrected Na = Measured Na + 1.6 × [(Glucose − 100) / 100]CorrectedNa=MeasuredNa+1.6×[(Glucose−100)/100]
Why This Matters in Nursing Practice
If corrected sodium is low:
- Patient has true sodium deficit
- May require isotonic saline continuation
If corrected sodium is normal/high:
- Switch to 0.45% saline
Understanding this calculation strengthens NCLEX electrolyte mastery and supports advanced nursing bundle decision-making.
3️⃣ Phosphate: The Silent Drop
Phosphate is often depleted in DKA due to osmotic diuresis.
During treatment:
- Insulin drives phosphate into cells
- Severe hypophosphatemia may develop
Why Nurses Should Care
Low phosphate can cause:
- Respiratory muscle weakness
- Difficulty weaning from ventilator
- Decreased cardiac contractility
- Hemolysis
Replacement is typically considered if:
- Phosphate <1.0 mg/dL
- Cardiac dysfunction present
- Respiratory compromise present
This is particularly important for ICU registered nurses managing ventilated patients.
4️⃣ Magnesium: The Overlooked Electrolyte
Magnesium is lost in osmotic diuresis and affects:
- Potassium regulation
- Cardiac electrical stability
- Neuromuscular function
Low magnesium makes potassium replacement ineffective.
Smart nursing care always checks magnesium if potassium remains unstable.
5️⃣ Bicarbonate: When Is It Used?
Routine bicarbonate use is not recommended.
Indications:
- pH <6.9
- Severe cardiovascular compromise
Improper bicarbonate administration may:
- Worsen intracellular acidosis
- Cause rapid potassium shifts
Another important NCLEX testing concept for the RN nurse.
ICU Electrolyte Monitoring Protocol
During active DKA treatment:
| Lab | Frequency |
|---|---|
| Blood glucose | Every 1 hour |
| Potassium | Every 2–4 hours |
| Sodium | Every 2–4 hours |
| Bicarbonate | Every 2–4 hours |
| Phosphate | Every 4–6 hours |
Continuous cardiac monitoring is mandatory.
This structured electrolyte approach forms a high-level nursing bundle for safe DKA resolution.
Nursing Complications to Watch For
As an experienced registered nurse, always anticipate:
- Hypokalemia → arrhythmias
- Cerebral edema (especially in pediatric patients)
- Hypoglycemia during insulin drip
- Rapid sodium shifts
- Fluid overload
Trend labs. Do not rely on a single value.
Resolution of DKA: When to Transition
DKA is considered resolved when:
- Blood glucose <200 mg/dL
- Bicarbonate ≥15 mEq/L
- pH >7.3
- Anion gap normalized
Even when glucose improves, electrolyte monitoring must continue.
This is another critical NCLEX testable principle.
High-Yield NCLEX Nursing Pearls
✔️ Potassium may look normal but is actually depleted
✔️ Never start insulin if potassium is <3.3 mEq/L
✔️ Use corrected sodium in hyperglycemia
✔️ Monitor labs every 2–4 hours
✔️ Hypophosphatemia can impair respiratory function
For every RN nurse, mastering electrolyte management in DKA separates task-based care from expert-level nursing practice.
Final Thoughts for the Nurse and Registered Nurse
Electrolyte monitoring during DKA treatment is dynamic and high risk. Insulin saves lives — but electrolyte mismanagement can end them.
Strong assessment skills, frequent lab review, and adherence to a structured nursing bundle ensure safe recovery.
Whether preparing for the NCLEX or managing patients in the ICU, mastering these electrolyte shifts makes you a safer, sharper, and more confident nurse.