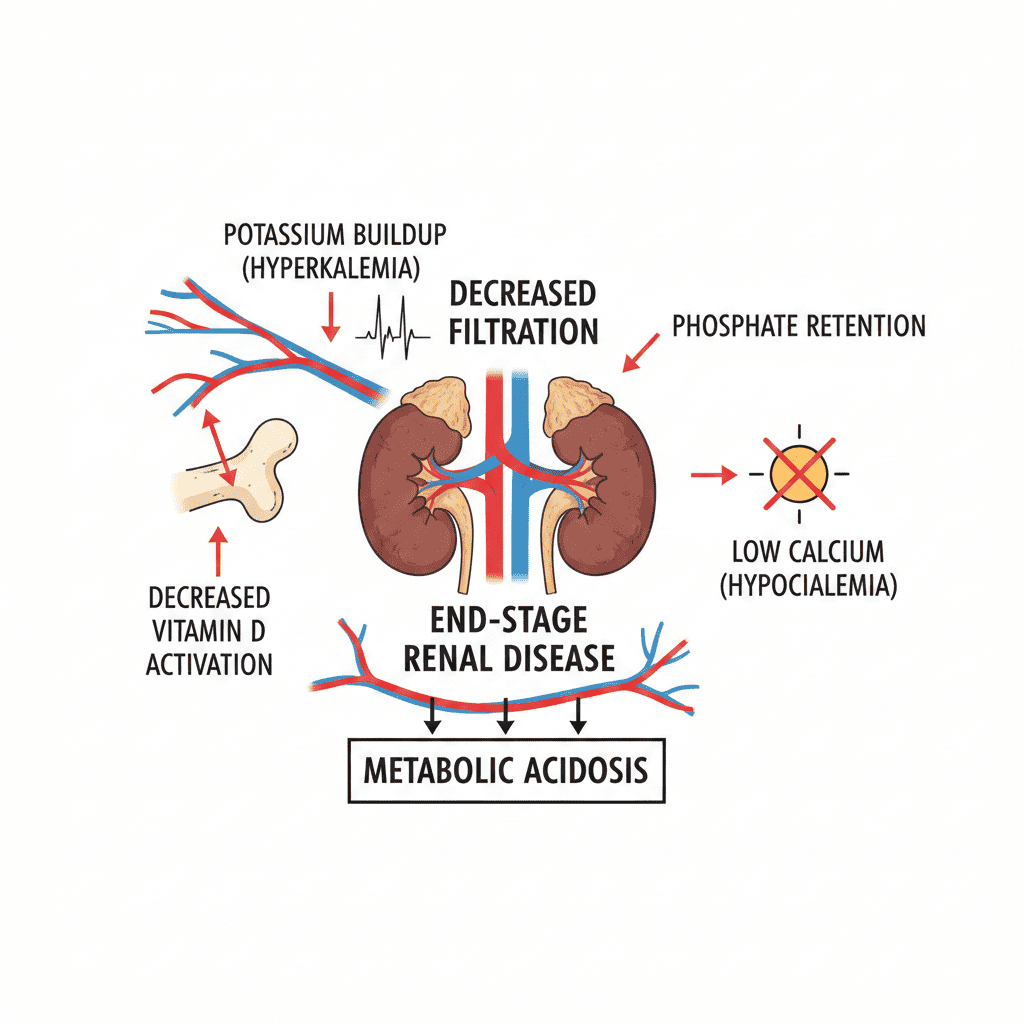
End-stage renal disease (ESRD) profoundly disrupts electrolyte balance, making it one of the most critical topics for any nurse, especially the dialysis or ICU registered nurse (RN nurse). Because the kidneys regulate sodium, potassium, calcium, phosphate, and acid-base balance, kidney failure results in complex, life-threatening imbalances. These disturbances are heavily tested on the NCLEX and frequently encountered in advanced nursing practice.
In end-stage renal disease, the kidneys lose the ability to excrete potassium, regulate sodium and water, activate vitamin D, and maintain acid-base balance — leading to dangerous electrolyte instability.
Why Electrolytes Become Unstable in ESRD
Healthy kidneys perform essential regulatory functions:
- Excrete excess potassium
- Control sodium and water balance
- Activate vitamin D
- Excrete phosphate
- Maintain bicarbonate levels
In ESRD (GFR <15 mL/min), these mechanisms fail.
The result: progressive electrolyte accumulation or depletion that directly affects cardiac, neurologic, and musculoskeletal systems.
For the RN nurse, understanding these mechanisms supports rapid clinical recognition.
Hyperkalemia: The Most Dangerous Disturbance
Why It Happens
The kidneys normally excrete potassium. In ESRD:
- Potassium accumulates
- Metabolic acidosis worsens potassium shift out of cells
Clinical Signs
- Muscle weakness
- Paresthesia
- Cardiac arrhythmias
ECG Changes (NCLEX Favorite)
- Peaked T waves
- Widened QRS
- Sine wave pattern
- Ventricular fibrillation
Hyperkalemia is a medical emergency.
The registered nurse must immediately report potassium levels >5.5 mEq/L and anticipate:
- IV calcium gluconate
- Insulin with dextrose
- Sodium bicarbonate
- Dialysis
Sodium and Fluid Imbalance
ESRD impairs sodium and water regulation.
Common Findings
- Fluid overload
- Hypertension
- Peripheral edema
- Pulmonary edema
Dilutional hyponatremia may occur due to excess water retention.
The nurse must:
- Monitor daily weights
- Assess lung sounds
- Monitor blood pressure
- Strictly track intake and output
Fluid assessment is a core dialysis nursing bundle component.
Metabolic Acidosis
The kidneys normally reabsorb bicarbonate and excrete hydrogen ions.
In ESRD:
- Acid accumulates
- Bicarbonate levels drop
- Metabolic acidosis develops
Effects
- Increased potassium levels
- Kussmaul respirations
- Fatigue
- Bone demineralization
On the NCLEX, metabolic acidosis is commonly linked with renal failure.
The RN nurse must monitor ABGs and serum bicarbonate.
Hyperphosphatemia
The kidneys excrete phosphate. In ESRD:
- Phosphate accumulates
- Calcium binds to phosphate
- Serum calcium decreases
This triggers secondary hyperparathyroidism.
Complications
- Bone disease (renal osteodystrophy)
- Vascular calcification
- Cardiovascular disease
Phosphate binders are often prescribed.
The registered nurse must ensure they are given with meals.
Hypocalcemia
Because kidneys activate vitamin D:
- Vitamin D decreases in ESRD
- Calcium absorption decreases
- Hypocalcemia develops
Symptoms
- Muscle cramps
- Tetany
- Prolonged QT interval
The RN nurse must monitor ECG changes and neuromuscular irritability.
Secondary Hyperparathyroidism
Low calcium + high phosphate stimulates parathyroid hormone (PTH).
Over time:
- Bone resorption increases
- Bones weaken
- Fracture risk increases
Understanding this hormonal chain is essential for advanced nursing care and NCLEX success.
Magnesium Imbalance
Magnesium is excreted by the kidneys.
In ESRD:
- Hypermagnesemia may develop
Signs
- Decreased reflexes
- Bradycardia
- Hypotension
The nurse must assess deep tendon reflexes in dialysis patients receiving magnesium-containing medications.
Dialysis and Electrolyte Shifts
Dialysis corrects:
- Hyperkalemia
- Fluid overload
- Acidosis
However, rapid shifts may cause:
- Hypotension
- Disequilibrium syndrome
- Muscle cramps
The registered nurse must monitor closely before, during, and after dialysis.
Cardiac Risks in ESRD
Electrolyte instability increases risk of:
- Ventricular arrhythmias
- Cardiac arrest
- Sudden death
Hyperkalemia remains the leading immediate threat.
Continuous cardiac monitoring is often necessary.
Nursing Bundle for ESRD Electrolyte Management
A structured ESRD nursing bundle should include:
1️⃣ Daily electrolyte monitoring
2️⃣ Continuous cardiac monitoring for high potassium
3️⃣ Strict intake/output tracking
4️⃣ Daily weights
5️⃣ Medication review (ACE inhibitors, potassium supplements)
6️⃣ Phosphate binder administration with meals
7️⃣ Patient education on dietary restrictions
Consistent monitoring prevents emergencies.
Diet and Patient Education
The RN nurse plays a critical role in teaching patients to limit:
- Potassium (bananas, oranges, tomatoes)
- Phosphate (dairy, processed foods)
- Sodium
- Fluids
Dietary compliance directly impacts survival in ESRD.
Education is frequently tested on the NCLEX.
NCLEX High-Yield Review
- ESRD causes hyperkalemia
- Peaked T waves = high potassium
- Kidneys activate vitamin D
- High phosphate → low calcium
- Metabolic acidosis increases potassium
- Dialysis removes potassium and fluid
If a dialysis patient presents with peaked T waves, suspect hyperkalemia immediately.
Integrating ESRD Knowledge into Nursing Practice
For the experienced registered nurse, electrolyte monitoring in ESRD is not optional — it is lifesaving.
Understanding the pathophysiology strengthens:
- Critical thinking
- ECG interpretation
- Dialysis care
- Emergency response
- NCLEX readiness
A proactive, structured nursing bundle approach improves outcomes and reduces cardiac complications.
Final Thoughts
Electrolyte disturbances in end-stage renal disease are complex, interconnected, and potentially fatal. Because the kidneys regulate nearly every major electrolyte, their failure creates systemic instability.
For every nurse and RN nurse, mastering these imbalances is essential for safe, effective nursing care and strong NCLEX performance.
Early recognition. Continuous monitoring. Rapid intervention.
That is the foundation of excellent renal nursing care.