Sodium imbalances are among the most common electrolyte disorders encountered in clinical practice. For every nurse, especially the registered nurse (RN nurse) working in acute care, understanding the cellular mechanisms behind sodium shifts is essential for safe patient management. Because hyponatremia and hypernatremia are heavily tested on the NCLEX, mastering the underlying physiology strengthens both exam performance and real-world nursing competence.
Sodium is not just a lab value — it directly affects cellular function, especially in the brain.
The Role of Sodium at the Cellular Level
Sodium (Na⁺) is the primary extracellular cation. It regulates:
- Fluid balance
- Osmolarity
- Nerve impulse transmission
- Muscle contraction
- Acid-base balance
Normal serum sodium range:
135–145 mEq/L
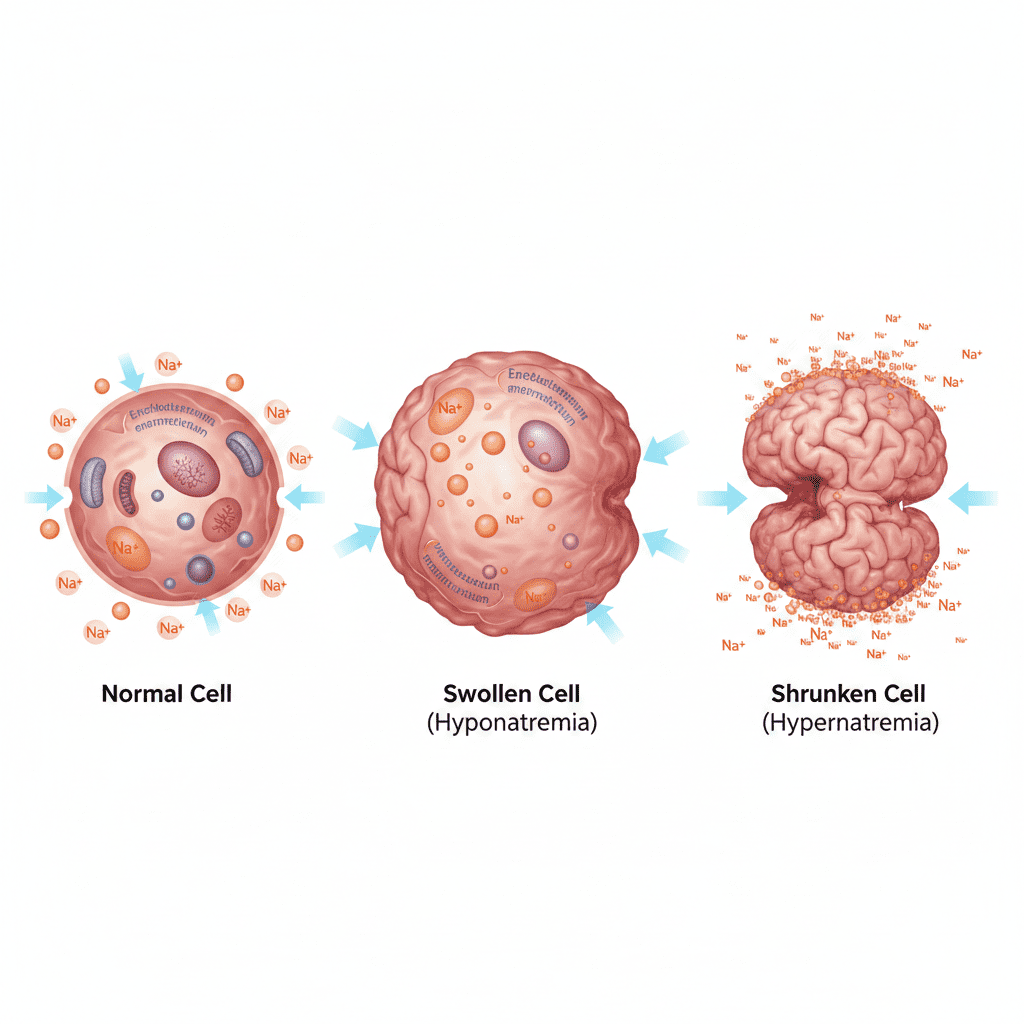
At the cellular level, sodium concentration determines the movement of water across cell membranes through osmosis.
Sodium imbalances cause water to shift in or out of cells, directly affecting cellular function—especially brain cells.
Sodium and Osmosis: The Core Mechanism
Water moves from areas of low solute concentration to areas of high solute concentration.
If sodium levels change in the bloodstream:
- Water shifts into cells → cellular swelling
- Water shifts out of cells → cellular shrinking
The brain is particularly sensitive because the skull limits expansion.
For the RN nurse, neurological assessment is critical in sodium disorders.
Cellular Mechanism of Hyponatremia
Hyponatremia occurs when serum sodium <135 mEq/L.
What Happens at the Cellular Level?
When sodium decreases in the blood:
- Extracellular fluid becomes hypotonic
- Water moves into cells
- Cells swell
In the brain, this leads to cerebral edema.
Causes of Hyponatremia
Common causes include:
- SIADH
- Heart failure
- Renal failure
- Excess free water intake
- Diuretics
On the NCLEX, SIADH is a classic cause of dilutional hyponatremia.
Cellular Effects in the Brain
Swelling of brain cells can cause:
- Headache
- Confusion
- Seizures
- Decreased level of consciousness
The registered nurse must monitor neurological status closely.
Rapid sodium decline is more dangerous than gradual changes.
Cellular Mechanism of Hypernatremia
Hypernatremia occurs when serum sodium >145 mEq/L.
What Happens at the Cellular Level?
When sodium increases in the blood:
- Extracellular fluid becomes hypertonic
- Water moves out of cells
- Cells shrink
Brain cells shrink, which may lead to vascular rupture in severe cases.
Causes of Hypernatremia
Common causes include:
- Dehydration
- Diabetes insipidus
- Excess sodium intake
- Inadequate water intake
On the NCLEX, diabetes insipidus is frequently associated with hypernatremia.
Adaptation Mechanisms of Brain Cells
The brain attempts to compensate for sodium imbalances.
In Hyponatremia:
Brain cells expel osmolytes to reduce swelling.
In Hypernatremia:
Brain cells generate osmolytes to retain water.
However, rapid correction disrupts this adaptation.
This is why slow correction is critical.
Risks of Rapid Sodium Correction
The RN nurse must understand:
Rapid Correction of Hyponatremia
Can cause Osmotic Demyelination Syndrome (ODS).
Rapid Correction of Hypernatremia
Can cause cerebral edema.
Safe correction rates are essential in advanced nursing care.
On the NCLEX, overcorrection is a dangerous clinical scenario.
Sodium and the Sodium-Potassium Pump
At the cellular level, the Na⁺/K⁺ ATPase pump:
- Moves sodium out of the cell
- Moves potassium into the cell
- Maintains electrical gradients
Sodium imbalances disrupt membrane potentials, affecting:
- Cardiac rhythm
- Muscle contraction
- Neurological signaling
The registered nurse must monitor ECG changes in severe imbalances.
Clinical Assessment for Nurses
When sodium imbalance is suspected, the RN nurse should assess:
- Level of consciousness
- Muscle strength
- Seizure activity
- Intake and output
- Fluid status
- Serum osmolality
Neurological changes are often the earliest sign.
Nursing Bundle for Sodium Imbalance Management
A structured nursing bundle improves patient safety:
- Frequent neurological assessment
- Strict intake and output monitoring
- Daily weights
- Lab trending
- Fluid restriction (if indicated)
- IV fluid management
- Seizure precautions (for severe hyponatremia)
Consistent monitoring prevents complications.
Treatment Principles
Hyponatremia
- Fluid restriction
- Hypertonic saline (severe cases)
- Treat underlying cause
Hypernatremia
- Gradual free water replacement
- Hypotonic IV fluids
- Treat underlying cause
The RN nurse must monitor correction rates closely.
NCLEX High-Yield Sodium Review
- Low sodium → cells swell
- High sodium → cells shrink
- Brain most affected
- Correct slowly
- Monitor LOC
- SIADH → hyponatremia
- Diabetes insipidus → hypernatremia
If a patient with hyponatremia develops confusion or seizures, prioritize airway and safety.
Integrating Cellular Knowledge Into Nursing Practice
Understanding cellular physiology enhances clinical judgment. The expert registered nurse does not simply treat lab numbers but understands the underlying mechanisms driving symptoms.
By applying a structured nursing bundle and consistent monitoring, nurses can:
- Prevent cerebral complications
- Improve patient outcomes
- Recognize early deterioration
- Enhance critical thinking
This deeper understanding also strengthens NCLEX preparation.
Final Thoughts
Sodium imbalances are more than electrolyte abnormalities — they are disruptions in cellular homeostasis that directly impact brain function. For every nurse and registered nurse, mastering the cellular mechanisms behind hyponatremia and hypernatremia is essential for safe, effective nursing care.
Because electrolyte management is heavily tested on the NCLEX, understanding water shifts, osmolarity, and brain adaptation strengthens both exam performance and bedside confidence.
In nursing practice, knowing what happens at the cellular level can prevent life-threatening complications.