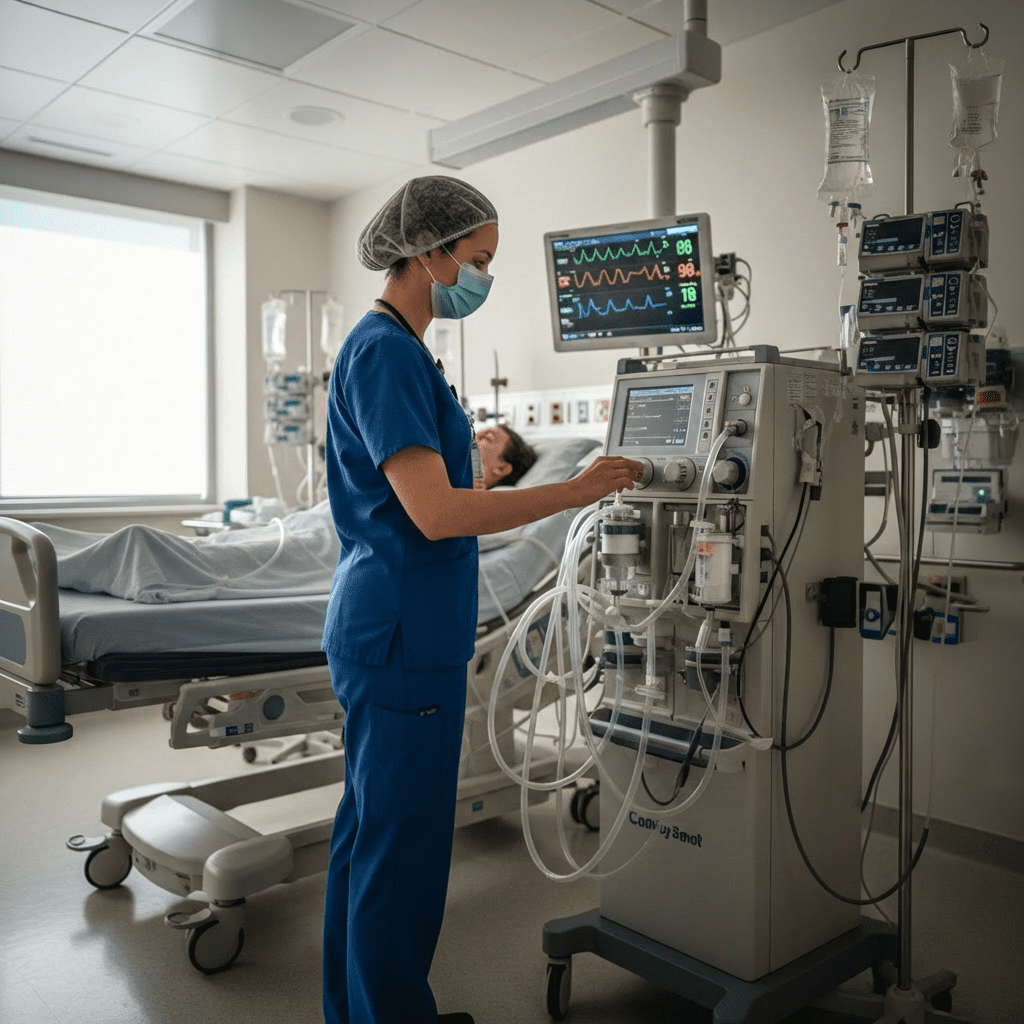
Continuous Renal Replacement Therapy (CRRT) is a life-saving intervention used in critically ill patients with acute kidney injury (AKI) who are hemodynamically unstable. For every nurse, especially the ICU registered nurse (RN nurse), understanding CRRT monitoring is essential for patient safety and optimal outcomes. Because fluid balance, electrolyte management, and renal failure are heavily tested on the NCLEX, mastering CRRT principles strengthens both exam preparation and real-world nursing competence.
CRRT requires precision, vigilance, and a structured nursing bundle approach to prevent complications.
What Is CRRT?
CRRT is a continuous dialysis modality performed over 24 hours, typically in the ICU.
It is preferred over intermittent hemodialysis when patients:
- Are hypotensive
- Require vasopressors
- Cannot tolerate rapid fluid shifts
- Have severe fluid overload
Unlike traditional dialysis, CRRT removes fluid and solutes slowly and steadily.
For the RN nurse, understanding this difference is critical.
Indications for CRRT
CRRT is initiated for:
- Acute kidney injury (AKI)
- Severe metabolic acidosis
- Hyperkalemia
- Fluid overload
- Uremia
- Septic shock with renal failure
On the NCLEX, hyperkalemia with ECG changes is a high-priority finding.
Types of CRRT Modalities
The registered nurse may encounter several CRRT modes:
1️⃣ CVVH (Continuous Venovenous Hemofiltration)
- Removes solutes by convection
2️⃣ CVVHD (Continuous Venovenous Hemodialysis)
- Removes solutes by diffusion
3️⃣ CVVHDF (Continuous Venovenous Hemodiafiltration)
- Combines convection and diffusion
Understanding the modality helps the RN nurse anticipate fluid and electrolyte changes.
Components of the CRRT Circuit
CRRT includes:
- Vascular access catheter (usually central line)
- Blood pump
- Filter (hemofilter)
- Dialysate fluid
- Replacement fluid
- Effluent collection bag
The nurse must ensure the circuit remains patent and functional at all times.
Nursing Monitoring Priorities During CRRT
CRRT requires continuous monitoring. The ICU nurse must assess:
- Vital signs
- Hemodynamic stability
- Fluid balance
- Electrolytes
- Circuit pressures
- Filter function
Strict hourly fluid balance monitoring is the most critical nursing responsibility during CRRT.
Fluid Balance Monitoring
CRRT removes fluid gradually.
The RN nurse must:
- Verify prescribed fluid removal rate
- Monitor intake and output hourly
- Assess for hypotension
- Adjust ultrafiltration per protocol
Excessive removal can cause:
- Hypotension
- Decreased perfusion
- Organ dysfunction
Fluid balance is a high-yield NCLEX concept.
Electrolyte Monitoring
CRRT significantly affects electrolyte levels.
The registered nurse must monitor:
- Potassium
- Sodium
- Calcium
- Magnesium
- Phosphorus
Hypokalemia and hypophosphatemia are common during CRRT.
On the NCLEX, electrolyte imbalances require immediate correction.
Anticoagulation in CRRT
To prevent filter clotting, anticoagulation is often required.
Common methods include:
- Heparin
- Citrate anticoagulation
Nursing responsibilities include:
- Monitoring aPTT (for heparin)
- Monitoring ionized calcium (for citrate)
- Watching for bleeding
Bleeding risk is a critical safety concern.
Recognizing CRRT Complications
The RN nurse must assess for:
Hypotension
- Most common complication
- Reduce ultrafiltration if needed
Filter Clotting
- Rising circuit pressures
- Frequent alarms
Electrolyte Imbalance
- Cardiac arrhythmias
- Muscle weakness
Infection
- Central line infection risk
Prompt recognition prevents deterioration.
CRRT Machine Alarms
CRRT machines generate alarms for:
- High access pressure
- High return pressure
- Air in line
- Filter clotting
The nurse must respond immediately and assess:
- Catheter position
- Blood flow rate
- Tubing kinks
On the NCLEX, equipment alarms should never be ignored.
Hemodynamic Monitoring
Patients on CRRT are often critically unstable.
The ICU registered nurse should monitor:
- MAP (goal ≥65 mmHg)
- Urine output
- Lactate
- Mental status
CRRT does not replace comprehensive shock management.
Lab Monitoring During CRRT
Typical labs monitored every 4–6 hours include:
- BMP
- ABGs
- Ionized calcium
- Magnesium
- Phosphorus
The nurse should trend labs and communicate abnormalities quickly.
Trending is an important NCLEX testing strategy.
CRRT Nursing Bundle Approach
A structured nursing bundle improves patient safety.
CRRT nursing bundle includes:
- Hourly intake/output documentation
- Frequent electrolyte monitoring
- Anticoagulation assessment
- Circuit pressure checks
- Central line care
- Hemodynamic monitoring
Consistency prevents complications.
Infection Prevention
CRRT requires central venous access.
The registered nurse must:
- Maintain sterile dressing changes
- Follow central line bundle protocols
- Assess for redness, swelling, drainage
- Monitor temperature
Central line-associated bloodstream infection (CLABSI) prevention is a nursing priority.
NCLEX High-Yield CRRT Review
- CRRT is continuous, slow dialysis
- Used for unstable patients
- Hourly fluid monitoring is critical
- Watch for hypotension
- Monitor potassium and phosphorus
- Assess for bleeding with anticoagulation
If a patient becomes hypotensive during CRRT, decrease fluid removal and assess immediately.
Prioritize perfusion.
Integrating CRRT Monitoring Into Nursing Practice
CRRT management requires advanced critical thinking skills. The experienced RN nurse must balance fluid removal, electrolyte stability, and hemodynamic support simultaneously.
By following a structured nursing bundle, ICU nurses can:
- Reduce complications
- Improve renal recovery
- Prevent electrolyte emergencies
- Enhance patient survival
CRRT exemplifies high-level critical care nursing expertise.
Final Thoughts
Continuous Renal Replacement Therapy is a complex but essential therapy for critically ill patients with renal failure. For every nurse and registered nurse, mastering CRRT monitoring is vital for patient safety.
Because fluid balance, renal function, and electrolyte management are frequently tested on the NCLEX, understanding CRRT strengthens both exam readiness and bedside confidence.
In critical care nursing, attention to detail saves lives — and CRRT demands nothing less.