Massive hemorrhage is a life-threatening emergency requiring rapid, coordinated intervention. For every nurse, especially the critical care registered nurse (RN nurse), understanding the Massive Transfusion Protocol (MTP) is essential for saving lives. Because hemorrhage management and shock are high-yield topics on the NCLEX, mastering MTP and coagulopathy management strengthens both exam preparation and real-world nursing practice.
Early recognition, rapid blood product administration, and correction of coagulopathy are the pillars of successful outcomes.
What Is Massive Transfusion?
Massive transfusion is typically defined as:
- Transfusion of ≥10 units of PRBCs within 24 hours
OR - ≥4 units in 1 hour with ongoing bleeding
It is commonly activated in:
- Trauma
- Obstetric hemorrhage
- GI bleeding
- Major surgery complications
- Ruptured aneurysm
The RN nurse must recognize early signs of exsanguination and activate the institutional nursing bundle promptly.
Pathophysiology of Trauma-Induced Coagulopathy
Massive bleeding leads to a deadly triad:
- Hypothermia
- Acidosis
- Coagulopathy
These factors worsen bleeding and increase mortality.
For the registered nurse, preventing this triad is a primary goal during MTP.
What Is the Massive Transfusion Protocol (MTP)?
MTP is a standardized emergency nursing bundle designed to rapidly deliver balanced blood components.
Most protocols use a 1:1:1 ratio:
- 1 unit PRBCs
- 1 unit Fresh Frozen Plasma (FFP)
- 1 unit Platelets
This mimics whole blood and prevents dilutional coagulopathy.
On the NCLEX, balanced transfusion ratios are frequently tested in trauma scenarios.
Indications to Activate MTP
The RN nurse should anticipate MTP activation if the patient shows:
- Hypotension
- Tachycardia
- Active uncontrolled bleeding
- Decreasing hemoglobin
- Altered mental status
- Signs of shock
Early activation improves survival.
Blood Products Used in MTP
Packed Red Blood Cells (PRBCs)
- Restore oxygen-carrying capacity
Fresh Frozen Plasma (FFP)
- Replaces clotting factors
Platelets
- Prevent thrombocytopenia
Cryoprecipitate
- Replaces fibrinogen
The registered nurse must verify blood products carefully and follow institutional transfusion safety protocols.
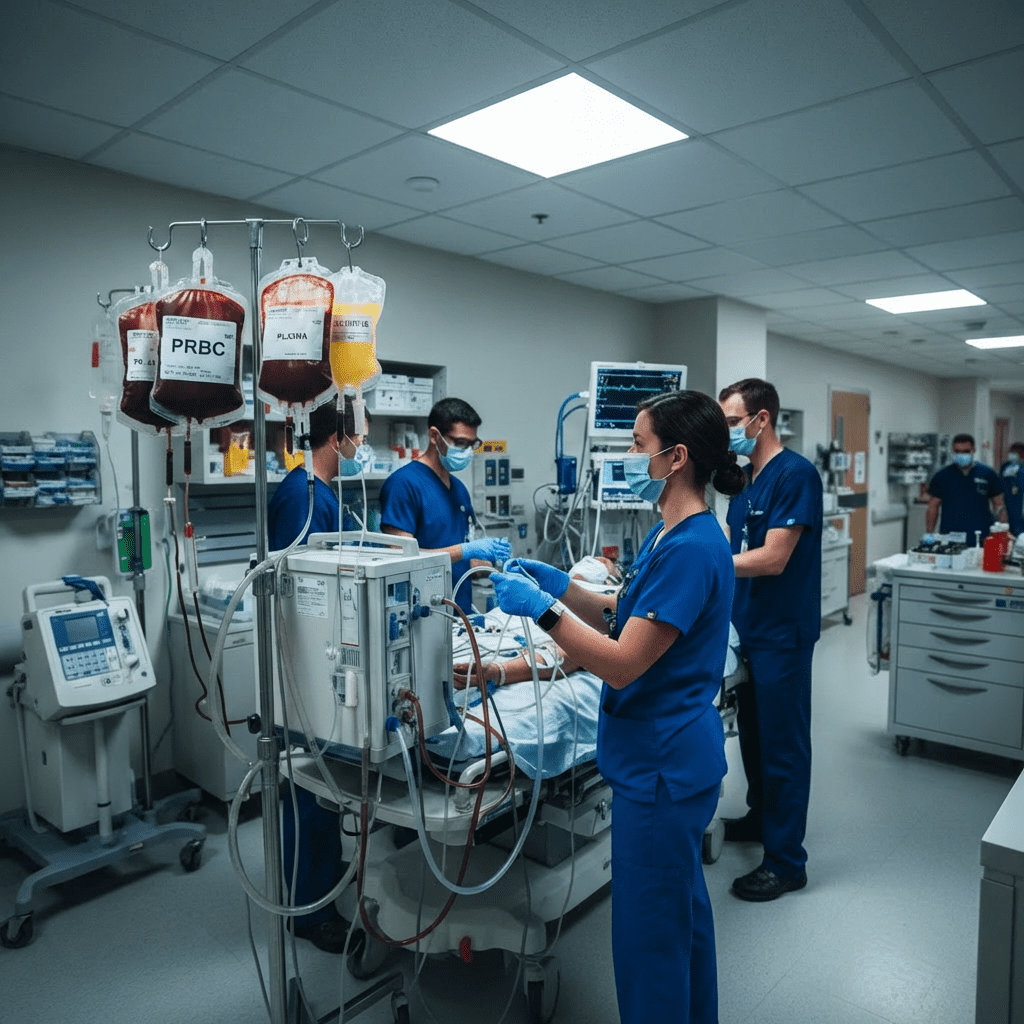
Nursing Responsibilities During MTP
The RN nurse plays a central role in:
- Rapid IV access (large-bore or central line)
- Use of rapid infuser device
- Continuous vital sign monitoring
- Monitoring transfusion reactions
- Accurate intake/output documentation
- Communication with blood bank
On the NCLEX, prioritization is key: airway, breathing, circulation always come first.
Balanced 1:1:1 transfusion during MTP prevents dilutional coagulopathy and improves survival in massive hemorrhage.
Monitoring for Coagulopathy
Massive transfusion can cause dilutional and consumptive coagulopathy.
Key labs to monitor:
- PT/INR
- aPTT
- Platelet count
- Fibrinogen level
- Lactate
- Hemoglobin
The nurse must trend lab values and report critical abnormalities immediately.
Preventing the Lethal Triad
1️⃣ Prevent Hypothermia
- Use blood warmers
- Apply warming blankets
- Monitor core temperature
Cold patients clot poorly.
2️⃣ Correct Acidosis
- Ensure adequate perfusion
- Administer fluids appropriately
- Monitor ABGs
Acidosis impairs clotting cascade function.
3️⃣ Manage Coagulopathy
- Administer plasma and platelets early
- Replace fibrinogen if low
- Follow lab-guided transfusion strategy
This structured approach functions as a life-saving nursing bundle.
Tranexamic Acid (TXA) in MTP
TXA helps stabilize clots by inhibiting fibrinolysis.
Key points for the RN nurse:
- Most effective within 3 hours of trauma
- Monitor for thromboembolic events
TXA use is commonly tested on the NCLEX in trauma patients.
Complications of Massive Transfusion
The registered nurse must monitor for:
- Transfusion reactions
- Hypocalcemia (due to citrate toxicity)
- Hyperkalemia
- Volume overload
- Acute lung injury (TRALI)
- Dilutional thrombocytopenia
Hypocalcemia signs include:
- Muscle twitching
- Hypotension
- Prolonged QT interval
Calcium replacement may be required.
Hemodynamic Monitoring During MTP
The RN nurse should continuously assess:
- Blood pressure
- Heart rate
- Urine output (≥0.5 mL/kg/hr)
- Mental status
- Capillary refill
Urine output is a key perfusion indicator — a common NCLEX testing point.
Documentation During MTP
Accurate documentation is critical in emergency nursing care.
Document:
- Time MTP activated
- Units transfused
- Vital signs
- Lab results
- Patient response
Clear documentation protects the RN nurse and improves interdisciplinary coordination.
NCLEX High-Yield Review
- Massive transfusion = ≥10 units PRBCs in 24 hours
- 1:1:1 ratio prevents coagulopathy
- Monitor for hypothermia and acidosis
- Watch for citrate-induced hypocalcemia
- Urine output indicates perfusion
If a trauma patient is hypotensive with active bleeding, anticipate MTP activation.
Prioritize circulation first.
Integrating MTP Into Nursing Practice
Massive hemorrhage management requires teamwork, speed, and clinical judgment. The skilled registered nurse coordinates blood administration, monitors for complications, and ensures safety throughout the process.
Following a structured nursing bundle approach improves:
- Survival rates
- Hemodynamic stability
- Prevention of coagulopathy
- Interdisciplinary efficiency
For every RN nurse in emergency or critical care settings, understanding MTP is essential.
Final Thoughts
Massive Transfusion Protocol is a life-saving intervention in patients experiencing severe hemorrhage. For the professional nurse and registered nurse, mastery of balanced transfusion, coagulopathy management, and complication monitoring is critical.
Because hemorrhage management is heavily emphasized on the NCLEX, understanding prioritization, lab interpretation, and transfusion safety strengthens both exam performance and bedside expertise.
In critical care nursing, rapid recognition and coordinated intervention can mean the difference between life and death.