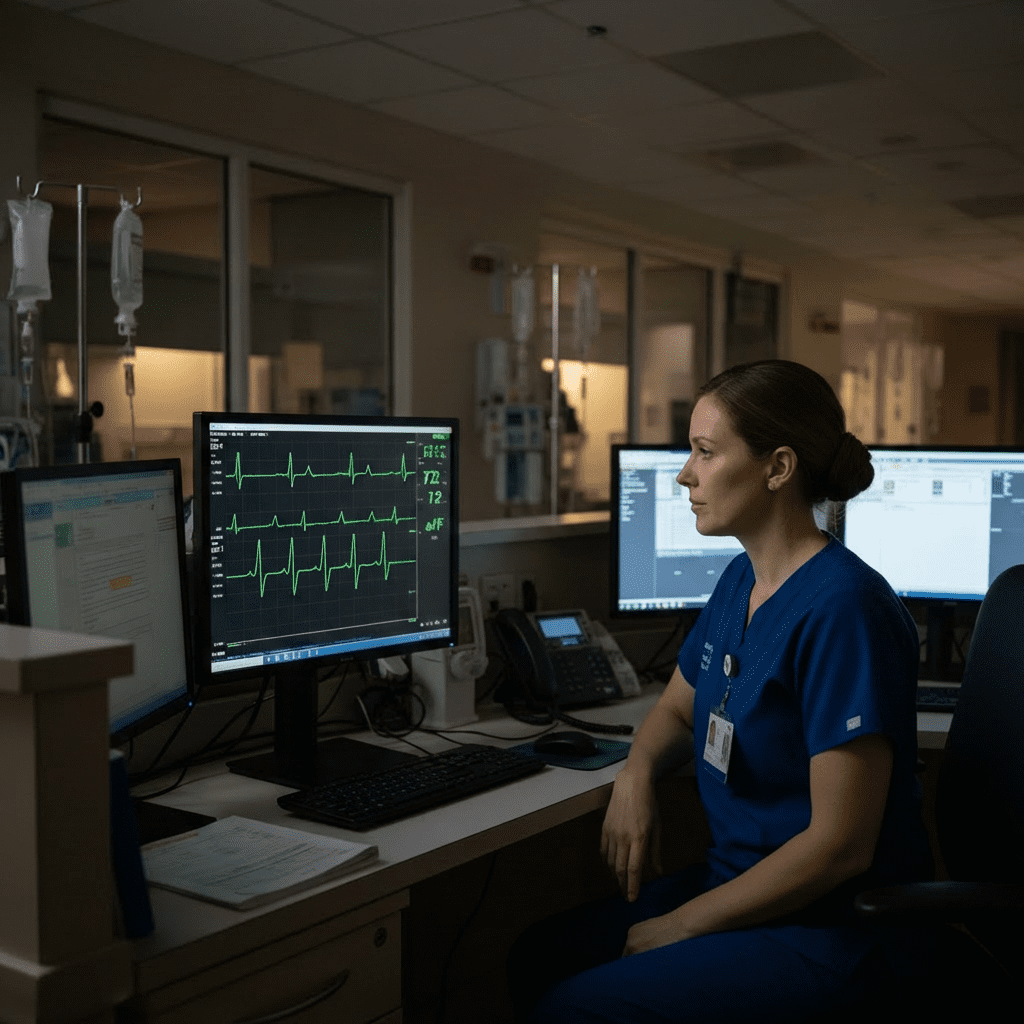
Night shifts bring unique challenges for every nurse, especially when monitoring cardiac telemetry. During nighttime hours, physiological changes, medications, sleep patterns, and reduced activity levels can all influence heart rhythms. For the registered nurse and RN nurse, recognizing these rhythm changes is essential for patient safety and NCLEX success. This guide explains the most common telemetry rhythm changes seen on night shift and highlights practical nursing actions.
Why Telemetry Rhythms Change at Night
At night, the body naturally shifts into a parasympathetic-dominant state. As a result, heart rate often slows, blood pressure decreases, and vagal tone increases. In addition, patients receive sedatives, sleep aids, pain medications, and nighttime doses of cardiac drugs. Because of these factors, telemetry alarms frequently activate during night shifts.
Therefore, the nurse must distinguish between expected physiologic changes and dangerous dysrhythmias.
Sinus Bradycardia: The Most Common Night Rhythm
Sinus bradycardia appears frequently during night-shift telemetry monitoring. In many patients, this rhythm reflects normal sleep physiology.
Key Features
- Heart rate below 60 bpm
- Regular rhythm
- Normal P waves before each QRS complex
Nursing Perspective
In stable patients, sinus bradycardia often requires monitoring only. However, the RN nurse should assess for dizziness, hypotension, altered mental status, or chest pain. If symptoms appear, prompt intervention becomes necessary.
💡 NCLEX Tip: Nighttime sinus bradycardia without symptoms is often expected, not an emergency.
Sinus Arrhythmia During Sleep
Sinus arrhythmia commonly appears during deep sleep, especially in younger or healthier patients. Respiratory patterns strongly influence this rhythm.
What You’ll See on Telemetry
- Irregular R-R intervals
- Normal P waves
- Rate varies with breathing
Nursing Actions
Instead of panicking, the nurse should correlate the rhythm with the patient’s respiratory pattern. Most of the time, no intervention is needed.
Atrial Fibrillation Rate Changes at Night
Patients with known atrial fibrillation often show rate slowing overnight. Medications such as beta-blockers and calcium channel blockers contribute to this effect.
Common Observations
- Slower ventricular response
- Irregularly irregular rhythm
- No distinct P waves
Nursing Focus
The registered nurse should watch for pauses, excessive bradycardia, or hypotension. Additionally, telemetry alarms may trigger repeatedly, which can lead to alarm fatigue if not managed properly.
Premature Atrial and Ventricular Contractions
PACs and PVCs frequently increase during night shifts due to electrolyte shifts, hypoxia, or medication timing.
Causes at Night
- Low potassium or magnesium
- Sleep apnea episodes
- Stress hormones fluctuating
- Reduced oxygen saturation
Nursing Response
Rather than ignoring frequent ectopy, the nurse should:
- Check electrolyte levels
- Assess oxygen status
- Review recent medications
This approach supports safe nursing care and prevents rhythm deterioration.
Heart Blocks: More Noticeable Overnight
First-degree and second-degree type I (Wenckebach) heart blocks often become more apparent during sleep.
Why This Happens
Increased vagal tone slows AV node conduction. As a result, PR intervals lengthen or dropped beats appear.
What the RN Nurse Should Do
If the patient remains asymptomatic, continued observation is usually sufficient. However, new-onset blocks or progression to higher-degree block require immediate provider notification.
💡 NCLEX Reminder: Nighttime Wenckebach can be benign, but context always matters.
QT Interval Changes on Night Shift
Electrolyte replacement often occurs overnight, especially potassium and magnesium. These replacements directly affect the QT interval.
Risks
- Prolonged QT increases torsades de pointes risk
- Rapid electrolyte infusions worsen instability
Nursing Priorities
The nurse should:
- Monitor QT interval trends
- Verify infusion rates
- Respond promptly to alarms
This knowledge is frequently tested on the NCLEX.
Alarm Fatigue: A Night-Shift Threat
Telemetry alarms increase at night due to benign rhythm changes. Unfortunately, constant alarms can desensitize staff.
Nursing Strategies
- Customize alarm limits per provider order
- Address underlying causes instead of silencing alarms
- Reassess lead placement regularly
Effective alarm management protects patients and supports safer nursing practice.
When to Worry: Red Flags on Night Shift
Although many rhythm changes are expected, some findings demand immediate action.
🚨 Concerning Telemetry Findings
- Symptomatic bradycardia
- New-onset atrial fibrillation
- Ventricular tachycardia
- Pauses longer than 3 seconds
- Sudden rhythm changes with hypotension
In these cases, the registered nurse must act quickly and escalate care.
NCLEX Focus: Night-Shift Telemetry Questions
The NCLEX often tests rhythm interpretation with contextual clues like “patient asleep” or “night shift assessment.”
Key Exam Tips
- Always assess the patient before the monitor
- Compare rhythm changes to baseline
- Prioritize symptomatic patients
- Know which rhythms are expected during sleep
Studying these concepts through a structured nursing bundle improves retention and exam confidence.
Final Thoughts for Nurses
Night-shift telemetry requires sharp assessment skills and strong clinical judgment. While many rhythm changes reflect normal physiology, others signal serious deterioration. By understanding common nighttime rhythms, the RN nurse improves patient safety and reduces unnecessary interventions.
For deeper mastery, combining telemetry practice with an EKG and Electrolyte Nursing Bundle provides targeted preparation for both bedside care and the NCLEX.